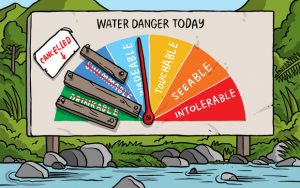
Potable water and the U.S. Centers for Disease Control: two things we take for granted.
 CDC reports that during 2013–2014, a total of 42 drinking water–associated outbreaks were reported, resulting in at least 1,006 cases of illness, 124 hospitalizations, and 13 deaths. Legionella was responsible for 57% of outbreaks and 13% of illnesses, and chemicals/toxins and parasites together accounted for 29% of outbreaks and 79% of illnesses. Eight outbreaks caused by parasites resulted in 289 (29%) cases, among which 279 (97%) were caused by Cryptosporidium and 10 (3%) were caused by Giardia duodenalis. Chemicals or toxins were implicated in four outbreaks involving 499 cases, with 13 hospitalizations, including the first outbreaks associated with algal toxins.
CDC reports that during 2013–2014, a total of 42 drinking water–associated outbreaks were reported, resulting in at least 1,006 cases of illness, 124 hospitalizations, and 13 deaths. Legionella was responsible for 57% of outbreaks and 13% of illnesses, and chemicals/toxins and parasites together accounted for 29% of outbreaks and 79% of illnesses. Eight outbreaks caused by parasites resulted in 289 (29%) cases, among which 279 (97%) were caused by Cryptosporidium and 10 (3%) were caused by Giardia duodenalis. Chemicals or toxins were implicated in four outbreaks involving 499 cases, with 13 hospitalizations, including the first outbreaks associated with algal toxins.
To provide information about drinking water–associated waterborne disease outbreaks in the United States in which the first illness occurred in 2013 or 2014 (https://www.cdc.gov/healthywater/surveillance/drinking-surveillance-reports.html), CDC analyzed outbreaks reported to the CDC Waterborne Disease and Outbreak Surveillance System through NORS (https://www.cdc.gov/nors/about.html) as of December 31, 2015. For an event to be defined as a waterborne disease outbreak, two or more cases must be linked epidemiologically by time, location of water exposure, and illness characteristics; and the epidemiologic evidence must implicate water exposure as the probable source of illness. Data requested for each outbreak include 1) the number of cases, hospitalizations, and deaths; 2) the etiologic agent (confirmed or suspected); 3) the implicated water system; 4) the setting of exposure; and 5) relevant epidemiologic and environmental data needed to understand the outbreak occurrences and for determining the deficiency classification.§ One previously unreported outbreak with onset date of first illness in 2012 is presented but is not included in the analysis of outbreaks that occurred during 2013–2014.
Public health officials from 19 states reported 42 outbreaks associated with drinking water during the surveillance period (Table 1) (https://www.cdc.gov/healthywater/surveillance/drinking-water-tables-figures.html).
One outbreak reported during 2013–2014 in an individual system led to 100 estimated illnesses associated with a wedding. The public health challenges highlighted here underscore the need for rapid detection, identification of the cause, and response when drinking water is contaminated by infectious pathogens, chemicals, or toxins to prevent and control waterborne illness and outbreaks.