Brazilian media report (via ProMed, thanks) that in the past 15 days, the number of cases of confirmed toxoplasmosis has increased from 594 to 621, according to a new epidemic bulletin from the government of Rio Grande do Sul and the city council on the epidemic facing the region.
 Of the more than 600 confirmed cases, 54 are pregnant women, with 3 fetal deaths and 3 abortions.
Of the more than 600 confirmed cases, 54 are pregnant women, with 3 fetal deaths and 3 abortions.
The number of suspected cases increased from 1291 on [29 Jun 2018] to 1486 on Friday. Of these, 350 were rejected and 515 arestill under investigation. The total number of cases related to the disease is 1786, according to the latest newsletter.
The causes of the epidemic, confirmed by the State Secretariat of SAR in April this year [2018], are still unknown, and the authorities continue to investigate the event, under the supervision of the federal prosecution. Last Friday [6 Jul 2018], an examination detected the presence of the protozoan responsible for the disease in the water tank of a town residence. But the relationship between the protozoan and the epidemic has not been confirmed.
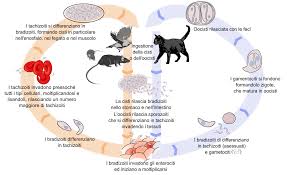
Toxoplasmosis, popularly known as cat disease, is an infectious disease caused by a protozoan called Toxoplasma gondii. This protozoan is easily found in nature and can cause infection in many mammals and birds around the world.
According to the Brazilian Society of Infectious Diseases, the disease can occur through the ingestion of oocysts (where the parasite grows) from soil, sand, and bins contaminated with feces from infected cats; ingestion of raw and undercooked meat infected with oocysts, especially pork and mutton; or by transplacental infection, occurring in 40% of fetuses of mothers who contracted infection during pregnancy. The incubation period of toxoplasmosis ranges from 10 to 23 days when the cause is meat consumption, and from 5 to 20 days when the reason is contact with cat feces oocysts.
The Brazilian Society of Infectious Diseases suggests some preventive measures. Do not eat raw or malnourished meats, and eat only well-washed vegetables and fruits cleaned with running water. Avoid contact with cat feces. In addition to avoiding contact with cats, pregnant women must undergo appropriate medical (prenatal) monitoring.









