The U.S. Centers for Disease Control, multiple states, and the U.S. Department of Agriculture Food Safety and Inspection Service (USDA-FSIS) are investigating a multistate outbreak of Shiga toxin-producing Escherichia coliO157:H7 (STEC O157:H7) infections.
 Seven people infected with the outbreak strain of STEC O157:H7 have been reported from four states.
Seven people infected with the outbreak strain of STEC O157:H7 have been reported from four states.
Five ill people have been hospitalized. No one has developed hemolytic uremic syndrome, a type of kidney failure, and no deaths have been reported.
Epidemiologic, traceback, and laboratory evidence indicate that beef products produced by Adams Farm Slaughterhouse in Athol, Massachusetts is a likely source of this outbreak.
On September 24, 2016, Adams Farm Slaughterhouse recalled beef, veal, and bison products due to possible E. coli O157:H7 contamination.
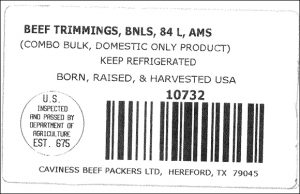
The products subject to recall have establishment number EST. 5497 inside the USDA mark of inspection and include several lot numbers and cuts of meat. The full list can be found on the USDA website.
These items were shipped to farmers’ markets, retail locations, and restaurants in Massachusetts, Connecticut, and eastern New York. The products may have been shipped to neighboring states.
We recommend that consumers, restaurants, and retailers do not use, serve, or sell the recalled meat products.
Don’t cook recalled meat products and eat them. Throw the meat out or return it to the place of purchase. If you throw it away, put it in a sealed bag in the trash so that children, pets, or other animals can’t eat it..
Public health investigators are using the PulseNet system to identify illnesses that may be part of this outbreak.
Illnesses started on dates ranging from June 27, 2016 to September 4, 2016. Ill people range in age from 1 year to 74, with a median age of 25. Fifty-seven percent of ill people are female. Five ill people have been hospitalized.
Epidemiologic, traceback, and laboratory evidence indicate that beef products produced by Adams Farm Slaughterhouse in Athol, Massachusetts is a likely source of this outbreak.
In interviews, ill people answered questions about the foods they ate and other exposures in the week before they became ill. All five (100%) of the five people reached for interview reported eating ground beef in the week before they became ill. Preliminary traceback information indicates that ill people ate ground beef which had been produced by Adams Farm Slaughterhouse.
The Connecticut Department of Public Health collected leftover ground beef from an ill person’s home and from a restaurant for testing; that beef had been produced by Adams Farm Slaughterhouse. Test results showed the outbreak strain of STEC O157:H7 in both samples of the leftover ground beef.
 The ground beef items were produced on August 19, 2016. The following products are subject to recall:
The ground beef items were produced on August 19, 2016. The following products are subject to recall: