MyNews LA reports a Downey man who falsely certified that beef being sold by his employer was free of E. coli bacteria — a lie that led to the recall of 5.7 million pounds of meat products — was sentenced Thursday to probation and home detention in what the judge called a “very difficult case.”
 Jim Johnson, a four-decade veteran of the beef industry who worked as a consultant to the now-defunct Huntington Meat Packing Co., was also ordered by U.S. District Judge Fernando M. Olguin to pay a share of $307,000 in restitution.
Jim Johnson, a four-decade veteran of the beef industry who worked as a consultant to the now-defunct Huntington Meat Packing Co., was also ordered by U.S. District Judge Fernando M. Olguin to pay a share of $307,000 in restitution.
Johnson, 68, pleaded guilty last year to a federal false-statements charge.
“There is no explanation for why he committed this crime,” Olguin said.
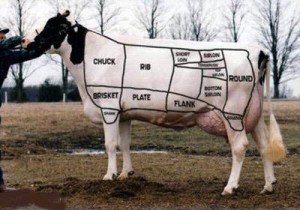
Huntington Meat was a Montebello-based meat processing and distribution company that sold raw ground beef used by other companies to make products such as beef patties and burrito mix. Under a food safety plan approved by the U.S. Department of Agriculture, Huntington Meat was required to test its products for safety.
Johnson admitted that in 2010, he knowingly and willfully provided the USDA’s Food Safety Inspection Service with a fake Certificate of Analysis, which falsely stated that a beef sample from the company had tested negative for E. coli.
Subsequent lab results showed some of that meat was contaminated with the bacteria, which prompted food regulators to issue the recall.
There were no illnesses linked to the recalled beef, according to the USDA.
“I am truly sorry for what I have done,” Johnson told the court. “I never meant to hurt anyone.”