A three-year-old girl from Dunbartonshire who died from E. coli O157 was among 20 confirmed cases that emerged in July and linked to Dunsyre Blue cheese made by South Lanarkshire-based Errington Cheese.
 On Saturday, Food Standards Scotland ordered the withdrawal from sale of batch G14 of Lanark White (unpasteurized) ewe milk cheese, adding, “A sample from a batch of Lanark White submitted for testing by South Lanarkshire Council has tested positive for E. coli O157. Although this organism may not carry shiga toxins, it is associated with human disease in the UK, so this cheese is a potential risk to health. FSS has issued a FAFA [Food Alert for Action] calling for this product to be immediately recalled from sale.”
On Saturday, Food Standards Scotland ordered the withdrawal from sale of batch G14 of Lanark White (unpasteurized) ewe milk cheese, adding, “A sample from a batch of Lanark White submitted for testing by South Lanarkshire Council has tested positive for E. coli O157. Although this organism may not carry shiga toxins, it is associated with human disease in the UK, so this cheese is a potential risk to health. FSS has issued a FAFA [Food Alert for Action] calling for this product to be immediately recalled from sale.”
The order to withdraw the cheese from sale was made after Errington refused to issue its own voluntary recall.
The company said the cheese had been on the market for three weeks with no reported cases of illness.
In a statement on its website, it said: “When we were told of the presumptive E. coli O157 result we immediately consulted experts in dairy microbiology.
“The experts told us they were confused and concerned by the testing methodology adopted by the laboratory.
“We have given careful consideration to this and to the fact that the cheese has been on the market for three weeks now with absolutely no reported incidence of illness.
“We have arranged for the sample of the same cheese tested by the authorities to be tested and the results will be ready on Monday when we will review the situation.”
Health Protection Scotland previously said that epidemiological investigations had “identified Dunsyre Blue cheese as the most likely cause of the outbreak”.
It added: “Despite extensive investigation, including looking for other possible food sources, no other link to a majority of cases could be established.”
Errington Cheese disputed the link, maintaining there was no conclusive evidence linking its products to the outbreak.
In a statement on its website last month it said that testing had shown it to be “completely clear of E. coli O157.”
Professor Hugh Pennington, the country’s leading expert on E. coli, told the Herald Scotland it could be difficult to identify it in any product suspected of causing food poisoning as by the time the illness comes to light, the food is usually all consumed or thrown away.
“Even if some of the batch (of food) is available for testing the bug might not be evenly distributed through a whole product, and so you might test part of the product that has been left or not been eaten yet and not find it – that doesn’t prove it wasn’t there in the bit that has been eaten,” he said.
“Scientifically it is sometimes quite complicated to come to a straightforward conclusion. The cheese manufacturers rightly say what is the evidence – but the regulatory authorities might never be able to come up with that.”
Joanna Blythman, investigative food journalist and the Sunday Herald’s food critic, said she believed there was a prejudice in Scotland against raw milk products, adding, “The (Dunsyre Blue) case puts a chill round everyone who wants to make a small scale artisan food. Meanwhile, the real prime suspects for large scale food poisoning are our industrial food producers.”
Stick to journalism. Illness per meal and type of food consumer and processing technique would have to be factored into any comparison of one food and artisan products.
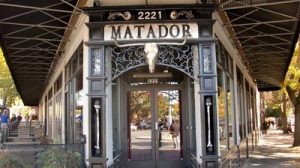
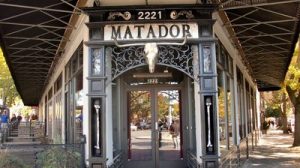
 33-year-old Annamarie Kirkpatrick said she ate at Matador in Seattle’s Ballard neighborhood on August 20. She became ill with severe abdominal pain five days later.
33-year-old Annamarie Kirkpatrick said she ate at Matador in Seattle’s Ballard neighborhood on August 20. She became ill with severe abdominal pain five days later.