I want a new drug, or approach or message, rather than CDC sending out yet another warning about yet another Salmonella outbreak from kids kissing their pet turtles.
 (And I can’t believe I’m quoting Huey Lewis and the News, one of my 1982 university room mates’ favorite bands, along with Hall and Oates).
(And I can’t believe I’m quoting Huey Lewis and the News, one of my 1982 university room mates’ favorite bands, along with Hall and Oates).
The U.S. Centers for Disease Control reports:
21 people infected with the outbreak strain of Salmonella Oranienburg have been reported from 13 states.
7 hospitalizations have been reported. No deaths have been reported.
Epidemiologic and traceback evidence indicate that contact with pet turtles is the likely source of this outbreak.
In interviews, 12 (71%) of 17 ill people reported contact with a turtle.
This investigation is ongoing and CDC will provide updates when more information is available.
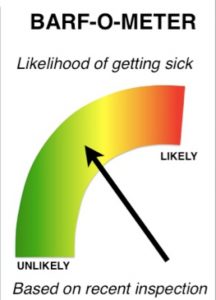
Turtles can carry Salmonella germs in their droppings while appearing healthy and clean. These germs can easily spread to their bodies, tank water, and habitats. People can get sick after they touch a turtle or anything in their habitats.
People who own or come in contact with turtles should take steps to stay healthy around their pet:
Wash your hands.
Always wash hands thoroughly with soap and water right after touching, feeding, or caring for a turtle or cleaning its habitat.
Adults should supervise handwashing for young children.
Play safely.
Don’t kiss or snuggle turtles, because this can spread Salmonella germs to your face and mouth and make you sick.
 Don’t let turtles roam freely in areas where food is prepared or stored, such as kitchens.
Don’t let turtles roam freely in areas where food is prepared or stored, such as kitchens.
Clean habitats, toys, and pet supplies outside the house when possible.
Avoid cleaning these items in the kitchen or any other location where food is prepared, served, or stored.
Pick the right pet for your family.
CDC and public health officials in several states are investigating a multistate outbreak of human Salmonella Oranienburg infections linked to contact with pet turtles.
Public health investigators are using the PulseNet system to identify illnesses that may be part of this outbreak. PulseNet is the national subtyping network of public health and food regulatory agency laboratories coordinated by CDC. DNA fingerprinting is performed on Salmonella bacteria isolated from ill people by using a standardized laboratory and data analysis method called whole genome sequencing (WGS). CDC PulseNet manages a national database of these sequences that are used to identify possible outbreaks. WGS gives investigators detailed information about the bacteria causing illness. In this investigation, WGS showed that bacteria isolated from ill people were closely related genetically. This means that people in this outbreak are more likely to share a common source of infection.
Ill people reported contact with red-eared sliders and other turtles that were larger than four inches in length. Previous Salmonella outbreaks have been linked to turtles with a shell length less than four inches. Due to the amount of Salmonella illnesses related to these small turtles, the U.S. Food and Drug Administration banned the sale and distributionexternal icon of turtles with shells less than four inches long as pets.
Regardless of where turtles are purchased or their size, turtles can carry Salmonella germs that can make people sick. Pet owners should always follow steps to stay healthy around their pet.
This investigation is ongoing, and CDC will provide updates when more information becomes available.