Elizabeth Weise in USA Today doesn’t really answer the who-should-pay question, but does ask, what if it were possible to almost entirely do away with E. coli in ground beef and it would cost only about a penny a burger?
Food-safety experts say it’s entirely feasible with new technologies that have become available. One is a vaccine, the other a feed additive, which, given early enough, could bring down potential E. coli contamination to negligible levels.
The problem, experts in beef safety say, is that the economics are backward. The new interventions have to be administered long before the cattle are slaughtered, when the calves are 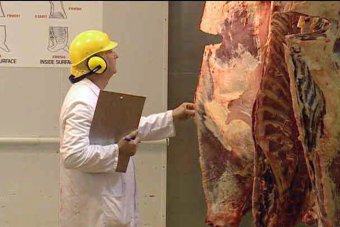 young or in feedlots where they’re growing.
young or in feedlots where they’re growing.
It’s hard to figure out who should pay for steps that would take place months and possibly years before the grill starts sizzling. The people who’d have to pay for them aren’t the ones who would reap the direct benefits.’’’
These interventions aren’t perfect, but they’re very good, says Guy Loneragan, a professor of food safety at Texas Tech University in Lubbock. "The question is no longer, ‘Can we get the technologies?’ We’ve got them, or they’re soon to arrive. The question is ‘How do we implement?’ "
So far only two small companies appear to be embracing them. One is a tiny feed lot cooperative in Kansas that’s looking to vaccinate all its cattle "soon." The other is a Meade, Kan., cooperative that’s staking its economic life on calling for retailers nationally to demand these interventions from the packers that supply their meat.
The regulatory landscape "is confusing," says Elisabeth Hagen, USDA’s undersecretary for food safety. "But we’re realizing that there’s an issue here and somehow we have to bring everybody together and focus on the end product, the result of which is the safety of the food that goes to the American consumer."
Loneragan says they’ve gone as far as they can after the animal is slaughtered. Now the focus needs to be on ridding the animals of E. coli O157:H7 before they get to the slaughterhouse. The new methods to do that involve:
•A vaccine. The biggest and potentially most game-changing treatment is a vaccine introduced by Pfizer Animal Health in 2010 and given in a three-shot series starting when the calf is just 6 months old. This gets rid of the E. coli O157:H7 bacteria in 85% of the cattle, says Brad Morgan, a senior food-safety specialist at Pfizer Animal Health in Stillwater, Okla. Not only that, but even among the ones that still have the bacteria in the gut, the injections reduce the amount the animals shed in their manure by 98%, he says.
It’s not all or nothing. Pfizer has done studies showing that if only 50% or even 25% of cattle are vaccinated, rates of E. coli are strongly reduced in the feed yard, and therefore in the packing plant. And Harvard’s Hammitt says his research shows that Americans understand that food can’t be "perfectly safe," but they want safer.
The vaccine costs $4 to $6 per animal for the full series, says Loneragan. There are several other vaccines in the regulatory pipeline here and overseas.
•The probiotic. The other intervention is a probiotic added to feed. These are beneficial bacteria cultures that out-compete the more dangerous forms of E. coli in the cattles’ guts, much as yogurt is said to seed the gut with good bacteria to keep out the bad. Many studies have .jpg) found that using "the right strain at the right dose you can get a fairly predictable 40% to 50% reduction in E. coli O157:H7," says Loneragan.
found that using "the right strain at the right dose you can get a fairly predictable 40% to 50% reduction in E. coli O157:H7," says Loneragan.
The American Meat Institute Foundation, the research arm of the meat industry trade group, says there just isn’t enough data yet to know if these treatments work. While there’s been a tremendous amount of research and it looks promising, "We’re right at the cusp of understanding the technology," says Betsy Booren, the institute’s director of scientific affairs.
Last year Cargill, one of the nation’s largest beef producers, conducted a trial of the E. coli vaccine on 85,000 head of cattle at its Fort Morgan, Colo., beef-processing facility, says spokesman Mike Martin at Cargill’s Wichita headquarters.
The trial’s results were "inconclusive," Martin says, in part because the levels of O157:H7 they found on the cattle in general "were the lowest in years . …" There was "very little difference" in rates between the vaccinated and the unvaccinated cattle, he says.
Loneragan says in the studies he’s done, E. coli O157:H7 levels were indeed low but dropped lower in meat from vaccinated cattle.
In the end, it’s going to take movement by the biggest companies to move the industry. There are two that could make this happen in a second, McDonald’s and Wal-Mart, says Chuck Jolley, a meat industry marketing company executive.
"If either decides to require it, the industry will turn around on a dime," he says.

 perhaps too graphic when compared to the histrionics that can be generated by hypothetical risks.
perhaps too graphic when compared to the histrionics that can be generated by hypothetical risks.

 "walk long distances or ride the bus" in order to sell it to restaurants.
"walk long distances or ride the bus" in order to sell it to restaurants.  a dollar per person each year, or an estimated $305 million in the aggregate, for a 10 percent reduction in the likelihood that hamburger they buy in the supermarket is contaminated by E. coli.
a dollar per person each year, or an estimated $305 million in the aggregate, for a 10 percent reduction in the likelihood that hamburger they buy in the supermarket is contaminated by E. coli. on the outside of the packet.
on the outside of the packet. beef and eggs, customers came back in a matter of weeks.
beef and eggs, customers came back in a matter of weeks..jpeg)
 Commerce subcommittee meeting today to the
Commerce subcommittee meeting today to the  Maryland regulators believed DeCoster eggs were such a threat that they banned sales of the eggs in their states.
Maryland regulators believed DeCoster eggs were such a threat that they banned sales of the eggs in their states. I’m also not a fan of whining.
I’m also not a fan of whining..jpg) On Friday, Amy made a stop at a local plant and produce shop to pick up a pumpkin.
On Friday, Amy made a stop at a local plant and produce shop to pick up a pumpkin. From the cider files
From the cider files