At least 90 British military personnel have been diagnosed with confirmed cases of Q fever after serving in Helmand, Afghanistan, a British court heard this week.
 According to a UK military news outlet, Forces Network, a consultant in infectious diseases and tropical medicine told the Central London Country Court on Tuesday that 90 confirmed cases of Q Fever had been recorded among British soldiers who had served in Helmand.
According to a UK military news outlet, Forces Network, a consultant in infectious diseases and tropical medicine told the Central London Country Court on Tuesday that 90 confirmed cases of Q Fever had been recorded among British soldiers who had served in Helmand.
Lieutenant Colonel Mark Bailey’s testimony was heard in the case of Wayne Bass, a private with 2nd Battalion the Mercian Regiment, who said his life has been ruined after he contracted the disease while in Helmand in 2011/2012.
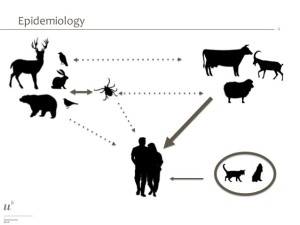
Humans can catch Q fever by breathing in dust from the feces of infected farm animals such as sheep, cattle and goats.
During his tour, his lawyers said Bass was in contact with goats and sheep and “was often required to take cover and jump through ditches and crawl along the ground – coming into contact with animal products and excrement”.
Bass, 34, was medically discharged from the Army in 2014 because of his Q fever and chronic fatigue symptoms.
Bailey, who specializes in infectious diseases and tropical medicine, and a national expert in Q fever, gave evidence during the second day of the trial.
Under questioning from Theo Huckle QC for Bass, Bailey said he has 90 military and 10 civilian cases in his care after they were referred to him.
He confirmed the 90 had served in Helmand and said the number of military cases “built up from 2008”, Forces Network reported.
Bailey told the court: “We have seen no new cases since 2014 from Afghanistan. Occasionally we get other military cases from other locations. Cyprus most recently.”
Bailey said he had seen “one British soldier who very, very nearly died” as a result of Q fever and subsequent complications, but there have been no UK deaths in his group.
In court documents setting out the case, it is argued that the MoD should have considered using Doxycycline, an antibiotic used to treat Q fever, as an anti-malarial drug, Forces Network reported.
The MoD however denies failing in its duty of care – pointing out that a vaccine used by some countries is not licensed in the UK.






 higher risk.
higher risk.