Maple Leaf Foods, the folks who made deli-meats that killed 23 Canadians in 2008, issued a public food safety pledge yesterday.
 Fearless and empathetic leader Michael McCain, speaking on behalf of the 23,500 employees of Maple Leaf Foods, said
Fearless and empathetic leader Michael McCain, speaking on behalf of the 23,500 employees of Maple Leaf Foods, said
“We have spent the last 18 months seeking the advice of the best experts in the world (and in many cases hiring them), examined every one of our previous practices, made significant improvements in all areas of food safety – testing, training and sanitization – and worked with industry and government to raise the bar.”
Maybe. But you’ve retained the worst public relations advisors and it’s going to take a lot of lemons to cleanse the stench on this pledge. Below are all the components of the frat-boy type pledge (thank you sir, may I have another) exactly as it appeared, even though it’s far too wordy, with some editorial comments from me.
*We commit to becoming a global leader in food safety. Our Chief Food Safety Officer will lead the implementation of best practices in sanitation, testing, technologies, product formulations and manufacturing, and has the authority to stop production at any plant where he believes there may be a risk to food safety.”
Awesome. Will those test results be made public?
*We commit to building a strong culture of food safety, with high performance teams, through continuous training, education and communicating results. Our people are  encouraged and expected to act on any food safety concern they may have to improve our food safety practices."
encouraged and expected to act on any food safety concern they may have to improve our food safety practices."
Communicating results, like making listeria test results public?
Public availability of food safety testing data underpins efforts to convince a skeptical public that a product is microbiologically safe.
Yes, testing has limitations, just like restaurant inspections, but the goal should be to figure out how best to make that information available – rather than saying people can’t have it or handle it.
On Dec. 31, 2009, Beef Products Inc. took a fairly public hit when the N.Y. Times questioned the efficacy of the company’s use of ammonia as an antimicrobial treatment for ground beef.
BPI founder and chairman Eldon Roth announced in February at the National Meat Association’s annual conference that the company will post on its Web site 100 per cent of its results from the processor’s testing for E. coli O157:H7 and salmonella.
"We’re going to be 100 percent transparent," Roth told Meatingplace in an interview following the announcement. … We’re not promising to be perfect, but I will promise that we will be better.”
That’s how it’s done.
*We commit to following the highest standard of testing and analysis to identify potential risk. Any test that raises food safety concerns will result in immediate quarantine, with no products leaving the plant until the Company (why is this capitalized? Is Maple Leaf its own nation-state? — dp) and government regulatory authorities are confident that the food is safe."
Test and hold. Sorta standard.
 *We commit to setting and meeting high standards and measuring our performance against the Global Food Safety Initiative standards through independent audits which will also allow us to continuously improve."
*We commit to setting and meeting high standards and measuring our performance against the Global Food Safety Initiative standards through independent audits which will also allow us to continuously improve."
Rather than relying on some auditor waltzing through the plant now and then, why not be able to prove how ab fab Maple Leaf is at this food safety thing. Borrow a page from Cargill (and activists around the world) and install your own video cameras to have data to support food safety pledges.
In April 2009, Cargill Beef announced it had implemented a third-party video-auditing system that would operate 24 hours a day at its U.S. beef plants to enhance the company’s animal welfare protection systems. All of Cargill’s U.S. plants were expected to have the program in place by the end of 2009.
In Feb. 2010, Cargill announced its expanded remote video auditing program will monitor food-safety procedures within its 10 beef-harvest facilities in North America.
Mike Siemens, Cargill leader of animal welfare and husbandry, said,
“The early results with our animal welfare program have been terrific and we’re excited to get all the facilities up-and-running on the program. Cargill has been able to use the RVA technology to help increase an already superior compliance rate at its plants to an even higher level. In addition to the positive results on compliance rates, we have observed healthy competition among plants on performance scores, as well as a general theme of collaboration among plants on how to attack specific operational challenges. The ability to share data and video easily is extremely valuable.”
Angie Siemens, Cargill technical services vice president for food safety and quality, said,
“We’re working to eliminate the opportunity for cross-contamination. We want to have the right steps at the beginning of our process to enhance the efficacy of our intervention technologies later in the process. The major objective of the video auditing application is to design a ground-breaking program that can further reduce the E. coli and Salmonella contamination.”
*We commit to openly sharing our knowledge with industry, government and consumers, so we can learn from them and they can learn from us, in pursuit of better food safety at every step of preparation."
 Your knowledge isn’t required. Data would be more meaningful. So would warning labels of some sort, especially for at-risk populations. Florida-based supermarket Publix places all of its deli-cut meats into a plastic bag that says:??
Your knowledge isn’t required. Data would be more meaningful. So would warning labels of some sort, especially for at-risk populations. Florida-based supermarket Publix places all of its deli-cut meats into a plastic bag that says:??
“The Publix Deli is committed to the highest quality fresh cold cuts & cheeses.
Therefore we recommend all cold cuts are best if used within three days of purchase.
And all cheese items are best if used within four days of purchase.”
*We commit to placing public interest and consumers first, by behaving in the most responsible and transparent way possible if there is ever a breach in our food safety system.”
Is that why Maple Leaf and the Canadian Food Inspection Agency set aside epidemiology and waited for confirmatory testing in an unopened package before issuing any public warning, even though local health units had already established a link with Maple Leaf products?
 Maple Leaf seems to be suffering from a common affliction that strikes many institutions in decline – they believe their own PR. Actions speak so much louder than words. From the beginning in Aug. 2008, Maple Leaf should have:
Maple Leaf seems to be suffering from a common affliction that strikes many institutions in decline – they believe their own PR. Actions speak so much louder than words. From the beginning in Aug. 2008, Maple Leaf should have:
• come clean on who knew what when regarding listeria testing;
• made listeria test results public;
• provided warning labels on deli meats for at-risk populations, like pregnant women and all those old people that unnecessarily died; and,
• marketed food safety efforts at retail so consumers can choose.
updates to its listeria control policy.
guidance on how to reduce the risks of acquiring listeriosis to personnel in institutions where high-risk people may be exposed.”

.jpg) household where a language other than English (LOTE) was spoken was the primary risk factor associated with listeriosis.
household where a language other than English (LOTE) was spoken was the primary risk factor associated with listeriosis.(3).jpeg) and preparation techniques.”
and preparation techniques.”(2).jpeg) cheeses soft-cooked eggs or sushi and sashimi.”
cheeses soft-cooked eggs or sushi and sashimi.”(2)(1).jpg) safe pregnancy options that don’t involve having to murder a meat dish that really should be served rare.
safe pregnancy options that don’t involve having to murder a meat dish that really should be served rare..jpg) "You don’t think about eating one piece of cheese and almost dying. That’s basically, what happened for both of us," said Stadler.
"You don’t think about eating one piece of cheese and almost dying. That’s basically, what happened for both of us," said Stadler.(2).jpg) The U.S. Centers for Disease Control and Prevention (CDC) has estimated approximately 2,500 cases of liisteriosis occur annually in the United States, with about 500 cases resulting in death. In 2000, listeria exposure resulted in a higher rate of hospitalization than any other foodborne pathogen and more than one-third of reported deaths from food pathogens.
The U.S. Centers for Disease Control and Prevention (CDC) has estimated approximately 2,500 cases of liisteriosis occur annually in the United States, with about 500 cases resulting in death. In 2000, listeria exposure resulted in a higher rate of hospitalization than any other foodborne pathogen and more than one-third of reported deaths from food pathogens..jpeg) mercury seafood (eg, salmon and shrimp) over higher mercury varieties (eg, fresh tuna). Pregnant women should ensure that their food is obtained from reputable establishments; stored, handled, and cooked properly; and consumed within a couple of days of purchasing.
mercury seafood (eg, salmon and shrimp) over higher mercury varieties (eg, fresh tuna). Pregnant women should ensure that their food is obtained from reputable establishments; stored, handled, and cooked properly; and consumed within a couple of days of purchasing. Fearless and empathetic leader Michael McCain, speaking on behalf of the 23,500 employees of Maple Leaf Foods,
Fearless and empathetic leader Michael McCain, speaking on behalf of the 23,500 employees of Maple Leaf Foods, Your knowledge isn’t required. Data would be more meaningful. So would warning labels of some sort, especially for at-risk populations. Florida-based supermarket Publix places all of its deli-cut meats into a plastic bag that says:??
Your knowledge isn’t required. Data would be more meaningful. So would warning labels of some sort, especially for at-risk populations. Florida-based supermarket Publix places all of its deli-cut meats into a plastic bag that says:?? Maple Leaf seems to be suffering from a common affliction that strikes many institutions in decline – they believe their own PR. Actions speak so much louder than words. From the beginning in
Maple Leaf seems to be suffering from a common affliction that strikes many institutions in decline – they believe their own PR. Actions speak so much louder than words. From the beginning in  That stood out for me in the
That stood out for me in the 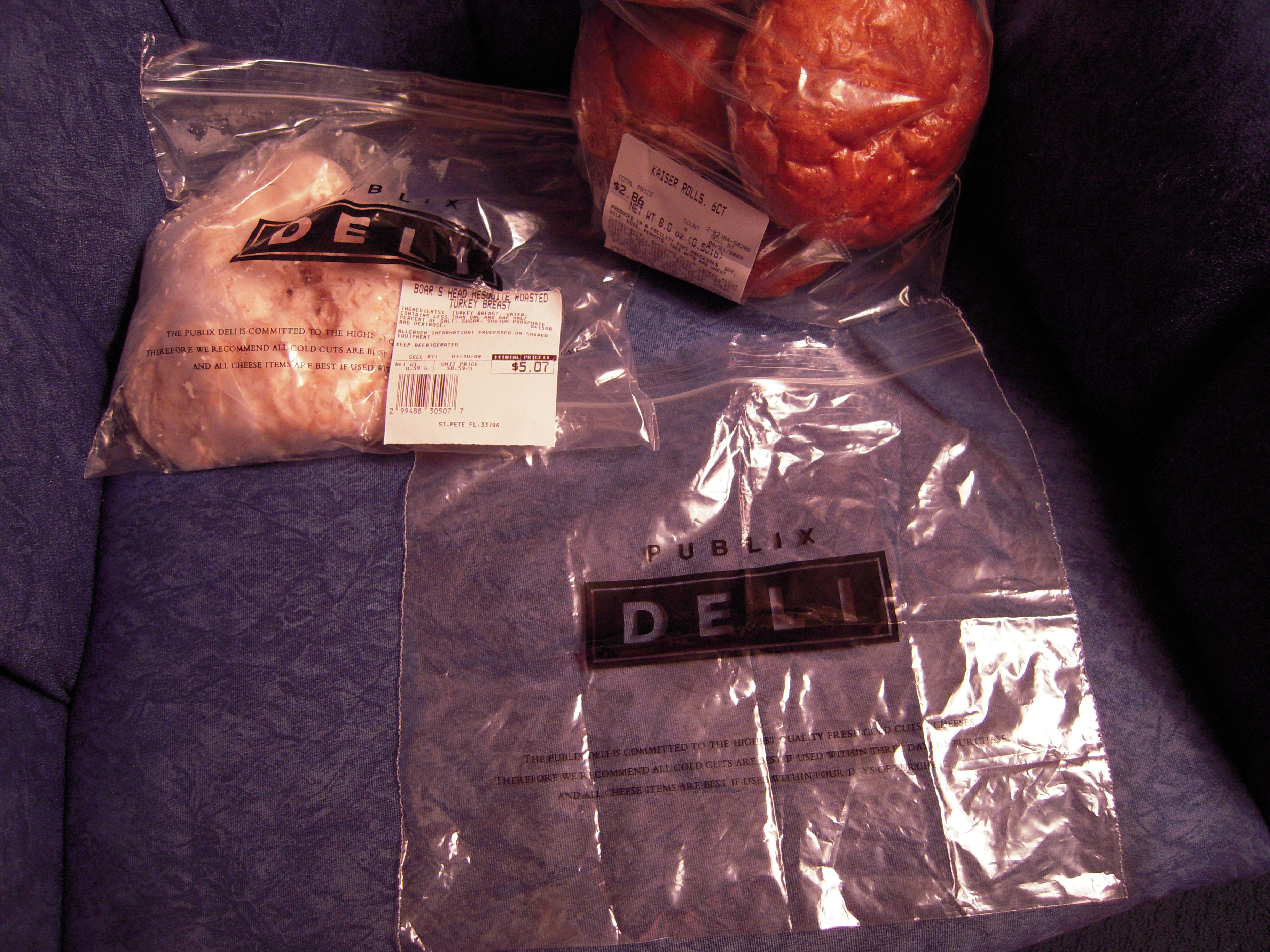 The stuff people buy in packages is safer, because of the antimicrobials approved for use in the U.S. and because those slicers are really hard to clean.
The stuff people buy in packages is safer, because of the antimicrobials approved for use in the U.S. and because those slicers are really hard to clean. of interest so assigned it to her translation class.
of interest so assigned it to her translation class. Two Oregon mothers have been sickened by listeria
Two Oregon mothers have been sickened by listeria