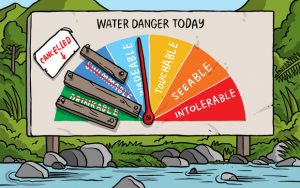
Tracy Watkins of Stuff writes complacency, inept officials – a Government inquiry paints a frightening picture of the state of New Zealand’s drinking water, with at least 750,000 of New Zealanders drinking from supplies that are “not demonstrably safe” – a figure described as likely to be a “significant underestimate.”
The inquiry was sparked by the 2016 Havelock North gastro outbreak, which has now been linked to four deaths, and calls for a major overhaul of water supplies, including mandatory treatment.
The Government has now written urgently to all mayors and district health boards asking to check the water they are supplying meets current standards after the inquiry revealed 20 per cent of water supplies were not up to standard.
That 20 per cent affects 759,000 people, of which 92,000 are at risk of bacterial infection, 681,000 of protozoal infection and 59,000 at risk from the long term effects of exposure to chemicals through their water supply.
But that figure was likely to understate the problem, as it did not include more than 600,000 people who drink water from self-suppliers or temporary suppliers, or tourists to places like Punakaiki on the West Coast, which is under a permanent “boil water” notice.
The inquiry found that complacency about the state of New Zealand’s drinking water was common, yet the evidence showed that in many cases it was safer to drink tap water overseas than here.
But its most damning findings related to the Ministry of Health, which it described as inept and negligent in its oversight of a system in which non-compliance with safe standards was high.
The risks for contamination of the water supplies were detailed by the inquiry including damaged pipes, a huge number of private and unknown bores, and the close proximity of sewerage to drinking water assets, a factor that caused surprise among overseas experts.
 The second part of the inquiry looked at broader water quality issues.
The second part of the inquiry looked at broader water quality issues.
It found that lessons from Havelock North appeared not to have been learned – compliance figures in the 2016-17 period were still “alarmingly low” and “do not appear to reflect any increased vigilance by suppliers in the aftermath of [that] outbreak”.
“The inquiry found the falling compliance levels with the bacteriological and chemical standards particularly concerning. The decrease in compliance with the bacteriological standards results from an increased number of transgressions, an increased number of supplies with ineffective, delayed or unknown remedial action following transgressions, and an increased number of supplies with inadequate monitoring.
“Twenty-seven supplies failed entirely to take any remedial action after a transgression. In the aftermath of the bacteriological outbreak in Havelock North, these failures to respond effectively to transgressions or to monitor adequately are surprising and unacceptable.”