Today is a state holiday in Queensland (that’s in Australia) as 60,000 or so will flock to the Ekka, the equivalent of a state fair.
 We’re not going.
We’re not going.
I got enough pictures the first two years, and wisely didn’t go last year when at least 50 were sickened with E. coli O157 linked to the animal displays.
Not a word about that outbreak from health types, fair types, or anyone, except locals who say, beware the Ekka winds, and wash hands.
The Minnesota Department of Health (MDH, that’s in the U.S.) has a much better history of identifying and following up on outbreaks, and reports today it has identified at least 13 people who have developed E. coli O157:H7 infections as part of an outbreak associated with Zerebko Zoo Tran traveling petting zoo. All of these cases have infections with E. coli O157:H7 bacteria that have the same DNA fingerprint. Two of these are secondary cases resulting from being exposed to one of the primary cases associated with the petting zoo.
The 13 cases range in age from 2 to 68 years, 10 (77 percent) are female, and they are residents of multiple counties. Seven (54 percent) cases have been hospitalized, including three children. Two of the cases developed a serious complication known as hemolytic uremic syndrome (HUS), which affects kidney function. Currently, one case is hospitalized with HUS.
The petting zoo exhibited at the events listed below between July 4 and July 27, and there have been cases associated with each one:
Nashwauk 4th of July Festival (7/3-7/5): 1 case
Polk County Fair (7/9-7/13): 1 case
Rice County Fair (7/15-7/20): 7 cases (including the 2 secondary cases)
Olmsted County Fair (7/21-7/27): 3 cases
MDH is currently following up with one case regarding their potential animal exposures prior to their illness. Additional cases associated with attending the Olmsted County Fair could still be identified, as that was the most recent event where Zerebko Zoo Tran exhibited.
 Environmental and animal fecal samples collected from Zerebko Zoo Tran yielded the outbreak strain of E. coli O157:H7. The owner has been cooperating in the investigation and voluntarily withheld his animals from the last two county fairs at which he was scheduled to exhibit in August.
Environmental and animal fecal samples collected from Zerebko Zoo Tran yielded the outbreak strain of E. coli O157:H7. The owner has been cooperating in the investigation and voluntarily withheld his animals from the last two county fairs at which he was scheduled to exhibit in August.
E. coli O157:H7 is commonly found in ruminant animals such as cattle, goats, and sheep. Outbreaks associated with these animals are documented virtually every year in Minnesota. Therefore, people who contact ruminants at any venue, public or private, are at risk for infection with E. coli O157:H7 as well as a variety of other germs. People typically become ill by getting bacteria on their hands after touching the animals or contaminated surfaces, and then swallowing the germs while eating, drinking or during other hand-to-mouth activities. Contamination can be present on the fur or in the saliva of animals, in the soil where these animals are kept, or on surfaces such as fence railings of animal pens.
“These illnesses are a stark reminder that E. coli O157:H7 can be present in even the cleanest of animal operations,” said MDH State Public Health Veterinarian Dr. Joni Scheftel. Risk associated with animal contact can be reduced through the following measures:
Visitors to animal exhibits should be made aware that even healthy, well-tended animals can have germs that can make people seriously ill.
Food, drinks, and items that promote hand-to-mouth contact (for example, pacifiers) should not be brought into animal areas.
Hands should be washed with soap and water immediately after visiting the animals. Hand sanitizers are not a substitute for soap and running water but may afford some protection until soap and water are available. They do not work well against some germs and when hands are visibly soiled.
Children under 5 years, seniors, pregnant women, and people with a chronic health condition or a weak immune system are prone to serious complications from E. coli infections and should take extra care around animals.
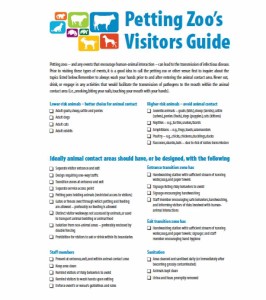
Best practices for planning events encouraging human-animal interactions
Zoonoses and Public Health
G. Erdozain , K. KuKanich , B. Chapman and D. Powell
http://onlinelibrary.wiley.com/doi/10.1111/zph.12117/abstract?deniedAccess
Educational events encouraging human–animal interaction include the risk of zoonotic disease transmission. It is estimated that 14% of all disease in the US caused by Campylobacter spp., Cryptosporidium spp., Shiga toxin-producing Escherichia coli (STEC) O157, non-O157 STECs, Listeria monocytogenes, nontyphoidal Salmonella enterica and Yersinia enterocolitica were attributable to animal contact. This article reviews best practices for organizing events where human–animal interactions are encouraged, with the objective of lowering the risk of zoonotic disease transmission.
A table of petting zoo outbreaks is available at https://barfblog.com/wp-content/uploads/2014/04/Petting-Zoo-Outbreaks-Table-4-8-14.xlsx.
 According to the Minnesota Department of Agriculture, two Minnesota residents sickened recently with salmonellosis are linked to frozen raw tuna, the Minnesota Department of Health (MDH) said today.
According to the Minnesota Department of Agriculture, two Minnesota residents sickened recently with salmonellosis are linked to frozen raw tuna, the Minnesota Department of Health (MDH) said today.