Posting a product recall (alert) notice on a company website, and then quickly removing it, is like putting down sugar to ward off ants. For the few remaining investigative journalists, such actions are akin to painting a bullseye on the company for further questioning.
 And it shouldn’t be that way.
And it shouldn’t be that way.
There is a scientific, public health and moral reason to make outbreaks known, whether product is still on the shelves or not. It’s how the rest of us mere mortals learn, it’s how to make things better, it’s the right thing to do.
Anyone who hides behind legalese is not worthy of trust – especially the consumer faith and trust that goes into every food purchase — because industry government, and academia rationalize a Chomsky-esque form of self-censorship that is barf-inducing to watch, and made worse by the Salmonella.
Coral Beach, formerly of The Packer and now with Bill Marler’s Food Safety News, reports that government and corporate entities failed to reveal in April that they were investigating a cluster of Salmonella illnesses in which at least five out of six victims reported eating Taylor Farms Organic Kale Medley Power Greens Mix purchased at various Sam’s Club locations.
After a notice on another company’s website — Pacific Coast Fruit Co. of Portland — brought the situation to light, Taylor Farms’ chairman and CEO Bruce Taylor confirmed that Minnesota officials had notified him about the investigation. However, it is not clear to whom Taylor issued his May 6 statement, which was still not available on the Taylor Farms website as of May 15.
Taylor’s statement, provided to Food Safety News on May 14, says:
 “On Thursday, May 5th, Taylor Farms was informed by the Minnesota Department of Health (MDH) and Minnesota Department of Agriculture (MDA) of an investigation of reported foodborne illness.
“On Thursday, May 5th, Taylor Farms was informed by the Minnesota Department of Health (MDH) and Minnesota Department of Agriculture (MDA) of an investigation of reported foodborne illness.
“In April, six people with Salmonella Enteritidis infections, with the same rare DNA fingerprint pattern, were reported to the MDH. All of those infected are from the state of Minnesota. All are recovering.
“The FDA is not requiring any action from Taylor Farms and we are not issuing any formal recalls. We will continue to work with the MDH and MDA regarding this issue.
“The safety and health of the consumers who buy our products has always and will always be the highest priority for us. We will continue to strive to deliver the industry highest quality, safest produce in the industry.”
Pleeeeassse.
Although Taylor did not reference a specific product or where it was distributed, the Pacific Coast Fruit Co. notice named Sam’s Club and said the retailer pulled Taylor Farms Organic Kale Medley Power Greens Mix from shelves nationwide on April 4.
The Pacific Coast Fruit notice, dated May 6, was available on the company’s website May 14, but has since been removed. The notice carried the headline “Taylor Farms-Organic Kale Medley Recall” and was addressed to “our customers and the Pacific Coast Fruit Team.”
Minnesota officials did not respond to weekend requests for comment on the situation. Similarly, no one from Pacific Coast Fruit or Sam’s Club responded this weekend to requests for comment.
The Pacific Coast Fruit notice said six people with Salmonella enteritidis infections, all with the same rare DNA fingerprint pattern, were reported to MDH in April. The victims ranged in age from 7 to 69 and their illnesses began between April 3 and April 26. One person was hospitalized, and all are recovering, according to Pacific Coast Fruit.
“Five of the ill people in Minnesota reported eating Taylor Farms Organic Kale Medley purchased at several Sam’s Club locations, and the source of the sixth person’s illness is under investigation,” Pacific Coast Fruit’s notice said.
An external communications spokesman for Taylor Farms said May 15 that the Salinas, CA, company did not need to issue a recall.
“No recall was needed because the issue being investigated was from back in late March early April. So, independent of the findings of the investigation, the product is no longer in the market place due to shelf-life limitations,” the Taylor Farms spokesman said.
 The failure of public health officials and corporate entities to announce the spike in Salmonella cases and the subsequent investigation is the latest incident in what one food safety professional says is a disturbing, decade-long trend.
The failure of public health officials and corporate entities to announce the spike in Salmonella cases and the subsequent investigation is the latest incident in what one food safety professional says is a disturbing, decade-long trend.
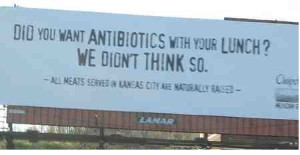
After the deadly E. coli outbreak in 2006 that was linked to bagged fresh spinach, companies have increasingly demanded governmental agencies provide confirmation results from time-consuming follow-up laboratory tests before issuing voluntary product recalls, said Douglas Powell, former professor at Kansas State University’s Department of Diagnostic Medicine/Pathobiology.
Powell, who now lives in Australia, is publisher of barfblog.com, which has been monitoring and publicizing foodborne illness outbreaks since 2006 (1993, when Food Safety Network started), coined the phrase “leafy green cone of silence” to describe the lack of transparency on the part of government and industry in the decade since the spinach outbreak.
“This situation fits the pattern,” Powell told Food Safety News May 15. “It’s part of a bigger picture about the question of when to go public about outbreak investigations.
“There’s a question of public health. I don’t care that the product’s not on the shelves any more. The public has a right and a need to know about these incidents.”
 Bill Marler, partner at the Seattle law firm Marler Clark LLP, had similar concerns. Marler has been representing victims of foodborne illnesses since the 1993 E. coli outbreak traced to undercooked hamburgers served by the Jack in The Box chain. He provided testimony to Congress during the drafting of the Food Safety Modernization Act.
Bill Marler, partner at the Seattle law firm Marler Clark LLP, had similar concerns. Marler has been representing victims of foodborne illnesses since the 1993 E. coli outbreak traced to undercooked hamburgers served by the Jack in The Box chain. He provided testimony to Congress during the drafting of the Food Safety Modernization Act.
“My main concern is the lack of transparency, and that’s not just a comment on Taylor Farms, it’s a comment on FDA, the Minnesota departments of health and agriculture and a comment on the CDC,” Marler said May 15. “I think that anytime, especially when there are illnesses involved, I think the public has an absolute right to know what’s going on.
“My assumption is that someone’s determined that the product is no longer in the marketplace because it’s a perishable product and the public’s no longer at risk. While I appreciate that, it’s not a reason to not let consumers know.
“In order for the free market to work, in order for consumers to know what products are safe or safer, the companies and the government have a responsibility to educate the consumer.
“When they withhold that kind of information, for whatever justifiable reason they think they have, it doesn’t give (consumers) the information to know how to protect themselves and their families and also calls into question public health’s commitment to the public’s health.”
 The recall involving the Gold’n Plump and Just Bare brands by the Upper Midwest’s leading chicken manufacturer follows the company disclosing the discovery of sand and black soil in the chicken. GNP is the parent of the popular Gold’n Plump brand.
The recall involving the Gold’n Plump and Just Bare brands by the Upper Midwest’s leading chicken manufacturer follows the company disclosing the discovery of sand and black soil in the chicken. GNP is the parent of the popular Gold’n Plump brand.