(although imperfect)
Those words, in parentheses, are the most important in a paper by CDC-types about self-reported consumption of pink beef, and impair the conclusions.
Researchers from the U.S. Centers for Disease Control used FoodNet data from a 2006-2007 survey of 8,543 respondents to conclude 75.3% reported consuming some type of ground beef in the home, and of those respondents who ate ground beef patties in the home, 18.0% reported consuming pink ground beef.
That’s a high number, but is pink hamburger correlated with cooking temperatures of less than 165F? Not always.
For purposes of the paper, pink hamburger is equated to undercooked and therefore potentially dangerous hamburger, except for the acknowledgement that color is an  “imperfect” indicator for the consumption of undercooked ground beef.
“imperfect” indicator for the consumption of undercooked ground beef.
The authors do mention in the paper that “color is not a reliable indicator of ground beef doneness, and thermometer use was not assessed so self-reported consumption of pink ground beef may not truly represent consumption of undercooked beef.
A series of studies beginning in the 1990s and led by Melvin “Hunter” Hunt of Kansas State University concluded that color is a lousy indicator of whether hamburger has reached a microbiologically safe internal temperature of 160F with something like 30 per cent of burgers browning prematurely, based on levels of different forms of myoglobin within hamburger. The U.S. Department of Agriculture agrees, and has a thorough summary of the problems with color at http://www.fsis.usda.gov/factsheets/Color_of_Cooked_Ground_Beef/index.asp.
So why base a consumer study on color, which research concludes and U.S. and Canadian governments agree in the form of consumer advice, is unreliable? Guess it was easier.
The survey did further verify a long-standing observation that is apparently ignored by every local, state or federal agency that says rates of E. coli O157:H7 increase in summer months because more people barbeque: there’s no correlation with cooking. Instead, the correlation is with microbial loads in cattle, which increase in spring and summer.
“We noted a distinct lack of seasonality in the consumption of ground beef or pink ground beef patties in the home. This contrasts with the marked seasonality reported for E. coli O157:H7 infections in humans, which peaks in the summer months. These data suggest that factors other than seasonality in ground beef consumption, such as differences in food handling practices or increases in the amount of bacterial contamination on meat and other foods or environmental sources during warmer months, are responsible for the seasonal increase in E. coli O157:H7 infections. Shedding of E. coli O157:H7 by cattle peaks during the spring and summer months, corresponding to the period of the highest incidence of human infections. Others have suggested that fluctuations in E. coli O157:H7 prevalence in cattle may be linked to human infections. Our data support this hypothesis and suggest that further attention to pre-harvest food safety interventions may be warranted to decrease the numbers of organisms shed in cattle feces and, ultimately, decrease the number of human infections."
For those who think consumers need to be better educated to reduce incidence of foodborne illness, the survey found yet another link to trash such a notion.
“Although persons with higher education and income reported consuming pink ground beef patties in the home more often, this group consumed ground beef overall less frequently. These findings do not explain these patterns, but we speculate that the increased level of risky behavior among more highly educated and higher income respondents may be due to several factors. These persons may not prepare food at home as often as other groups and
.jpg) therefore may be less practiced in appropriate safe food handling and cooking practices or they may prefer pink ground beef. Higher income persons have been shown both to have more confidence in the safety of the national food supply and to be more likely to use unsafe food practices than lower income persons. Persons that are more educated may also perceive themselves to be at less risk for foodborne illness and consequently be more likely to engage in risky behaviors. The increased willingness among this population to engage in unsafe food-related behaviors has been suggested to rise from more prevalent beliefs that they understand and can control food safety risks.”
therefore may be less practiced in appropriate safe food handling and cooking practices or they may prefer pink ground beef. Higher income persons have been shown both to have more confidence in the safety of the national food supply and to be more likely to use unsafe food practices than lower income persons. Persons that are more educated may also perceive themselves to be at less risk for foodborne illness and consequently be more likely to engage in risky behaviors. The increased willingness among this population to engage in unsafe food-related behaviors has been suggested to rise from more prevalent beliefs that they understand and can control food safety risks.”
Or, smart people can be dumb. Certainly applies to me (the dumb part).
The abstract of the paper is below.
Ground beef consumption patterns in the United States, FoodNet, 2006 through 2007
Journal of Food Protection®, Volume 75, Number 2, February 2012 , pp. 341-346(6)
Taylor, Ethel V.; Holt, Kristin G.; Mahon, Barbara E.; Ayers, Tracy; Norton, Dawn; Gould, L. Hannah
http://www.ingentaconnect.com/content/iafp/jfp/2012/00000075/00000002/art00016/
Infection resulting from foodborne pathogens, including Escherichia coli O157:H7, is often associated with consumption of raw or undercooked ground beef. However, little is known about the frequency of ground beef consumption in the general population. The objective of this study was to describe patterns of self-reported ground beef and pink ground beef consumption using data from the 2006 through 2007 FoodNet Population Survey. From 1 July 2006 until 30 June 2007, residents of 10 FoodNet sites were contacted by telephone and asked about foods consumed within the previous week. The survey included questions regarding consumption of ground beef patties both inside and outside the home, the consumption of pink ground beef patties and other types of ground beef inside the home, and consumption of ground beef outside the home. Of 8,543 survey respondents, 75.3% reported consuming some type of ground beef in the home. Of respondents who ate ground beef patties in the home, 18.0% reported consuming pink ground beef. Consumption of ground beef was reported most frequently among men, persons with incomes from $40,000 to $75,000 per year, and persons with a high school or college education. Ground beef consumption was least often reported in adults ≥65 years of age. Men and persons with a graduate level education most commonly reported eating pink ground beef in the home. Reported consumption of ground beef and pink ground beef did not differ by season. Ground beef is a frequently consumed food item in the United States, and rates of consumption of pink ground beef have changed little since previous studies. The high rate of consumption of beef that has not been cooked sufficiently to kill pathogens makes pasteurization of ground beef an important consideration, especially for those individuals at high risk of complications from foodborne illnesses such as hemolytic uremic syndrome.

.jpg) six months prior to the inspection, when six mice were exterminated.
six months prior to the inspection, when six mice were exterminated..jpg)
 and unpasteurized milk, the political history of raw milk in America and in Kansas, and how to find quality sources of raw milk for you and your family. … this class is essential for all people who want a healthy lifestyle.”
and unpasteurized milk, the political history of raw milk in America and in Kansas, and how to find quality sources of raw milk for you and your family. … this class is essential for all people who want a healthy lifestyle.” raw milk and dairy products because they may contain pathogenic bacteria that can make them sick.
raw milk and dairy products because they may contain pathogenic bacteria that can make them sick.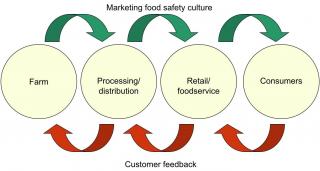
.jpg) regulations and inspections, or their food safety culture, is often overlooked.
regulations and inspections, or their food safety culture, is often overlooked..jpg) Department of Agriculture and the cooperation of the Sacred Heart Catholic Church in Arkansas City, have been conducting an investigation of a foodborne illness outbreak associated with the Sacred Heart Turkey Dinner that was held on the evening of November 8.
Department of Agriculture and the cooperation of the Sacred Heart Catholic Church in Arkansas City, have been conducting an investigation of a foodborne illness outbreak associated with the Sacred Heart Turkey Dinner that was held on the evening of November 8. (1).jpg) the Sacred Heart Catholic Church in Arkansas City, are continuing to conduct an investigation of a possible foodborne illness outbreak, and are asking for the public’s help in completing a survey to identify the source of the outbreak.
the Sacred Heart Catholic Church in Arkansas City, are continuing to conduct an investigation of a possible foodborne illness outbreak, and are asking for the public’s help in completing a survey to identify the source of the outbreak.  possible foodborne illness outbreak associated with the Sacred Heart Turkey Dinner that was held on the evening of November 8.
possible foodborne illness outbreak associated with the Sacred Heart Turkey Dinner that was held on the evening of November 8.  washing their hands, bare hand contact with ready-to-eat food during preparation, improperly sanitizing food contact and preparation areas, and improper cold holding temperatures.
washing their hands, bare hand contact with ready-to-eat food during preparation, improperly sanitizing food contact and preparation areas, and improper cold holding temperatures. violations including improper cold holding temperatures, improperly storing chemicals above food preparation areas, and improperly cleaning and sanitizing food contact surfaces.
violations including improper cold holding temperatures, improperly storing chemicals above food preparation areas, and improperly cleaning and sanitizing food contact surfaces. temperatures, improperly storing chemicals near food preparation areas, and improperly marking dates on food packages; sliced tomatoes and tuna salad were stored in a cooler at almost 60 degrees.
temperatures, improperly storing chemicals near food preparation areas, and improperly marking dates on food packages; sliced tomatoes and tuna salad were stored in a cooler at almost 60 degrees.