Snappy title, eh? But not bad for a peer-reviewed journal article in Food Control that was published on-line today ahead of print publication.
Almost two decades ago, E. coli O157:H7 killed four and sickened hundreds who ate hamburgers at the Jack-in-the-Box fast-food chain in the U.S. and propelled microbial food safety to the forefront of the public agenda. (1).jpg) However, it remains a challenge to compel food producers, processors, distributors, retailers, foodservice outlets and home meal preparers to adopt scientifically validated safe food handling behaviors, especially in the absence of an outbreak.
However, it remains a challenge to compel food producers, processors, distributors, retailers, foodservice outlets and home meal preparers to adopt scientifically validated safe food handling behaviors, especially in the absence of an outbreak.
Readers of barfblog.com will be familiar with the details surrounding the three case studies of failures in food safety culture documented in the paper: E. coli O157:H7 linked to John Tudor & Son in Wales in 2005; listeria linked to cold-cuts produced by Maple Leaf Foods of Canada in 2008; and salmonella linked to Peanut Corporation of America in 2009.
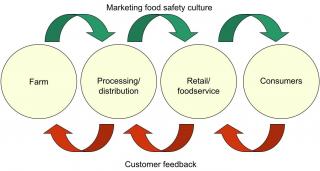
But anyone can be a critic, so we offer suggestions to enhance food safety culture, such as food safety storytelling through infosheets (Chapman, et al., 2010). And we end with my usual plea to actively promote food safety efforts, coupling a strong food safety culture with marketing to the world.
We conclude:
Creating a culture of food safety requires application of the best science with the best management and communication systems. It requires commitment by an organization’s leaders, middle managers and food handlers. It also must be supported and demonstrated by sharing information within the organization and with customers. The food safety failures of John Tudor & Sons, Maple Leaf Foods, Inc. and PCA are illustrative of an emerging recognition that the culture of food safety within an organization is a significant risk factor in foodborne illness (Griffith et al., 2010a; Yiannis, 2009).
Individuals focusing on food safety risks within an organization with a good food safety culture:
• know the risks associated with the foods they handle and how those should be managed;
• dedicate resources to evaluating supplier practices;
 • stay up-to-date on emerging food safety issues;
• stay up-to-date on emerging food safety issues;
• foster a value system within the organization that focuses on avoiding illnesses;
• communicate compelling and relevant messages regarding risk reduction activities and empower others to put them into practice;
• promote effective food safety systems before an incident occurs; and,
• do not blame customers (including commercial buyers and end consumers) when illnesses are linked to their products.
The best food producers, processors, retailers and restaurants should go above and beyond minimal government and auditor standards and sell food safety solutions directly to the public. The best organizations will use their own people to demand ingredients from the best suppliers; use a mixture of .jpg) encouragement and enforcement to foster a food safety culture; and use technology to be transparent – whether it’s live webcams in the facility or real-time test results on the website – to help restore the shattered trust with the buying public.
encouragement and enforcement to foster a food safety culture; and use technology to be transparent – whether it’s live webcams in the facility or real-time test results on the website – to help restore the shattered trust with the buying public.
I’ll add more as the paper becomes available, and if Chapman has anything witty to add (that takes time).
Enhancing food safety culture to reduce rates of foodborne illness
Douglas A. Powella, Casey J. Jacoba and Benjamin J. Chapmanb,
a Department of Diagnostic Medicine/Pathobiology, Kansas State University, Manhattan, KS 66506, USA
b Department of 4-H Youth Development and Family and Consumer Sciences North Carolina State University, Campus Box 7606, Raleigh, NC 27695-7606, USA
Received 2 August 2010;
revised 29 November 2010;
accepted 7 December 2010.
Available online 24 December 2010.
Abstract
A culture of food safety is built on a set of shared values that operators and their staff follow to produce and provide food in the safest manner. Maintaining a food safety culture means that operators and staff know the risks associated with the products or meals they produce, know why managing the risks is important, and effectively manage those risks in a (1)(1).jpg) demonstrable way. In an organization with a good food safety culture, individuals are expected to enact practices that represent the shared value system and point out where others may fail. By using a variety of tools, consequences and incentives, businesses can demonstrate to their staff and customers that they are aware of current food safety issues, that they can learn from others’ mistakes, and that food safety is important within the organization. The three case studies presented in this paper demonstrate that creating a culture of food safety requires application of the best science with the best management and communication systems, including compelling, rapid, relevant, reliable and repeated food safety messages using multiple media.
demonstrable way. In an organization with a good food safety culture, individuals are expected to enact practices that represent the shared value system and point out where others may fail. By using a variety of tools, consequences and incentives, businesses can demonstrate to their staff and customers that they are aware of current food safety issues, that they can learn from others’ mistakes, and that food safety is important within the organization. The three case studies presented in this paper demonstrate that creating a culture of food safety requires application of the best science with the best management and communication systems, including compelling, rapid, relevant, reliable and repeated food safety messages using multiple media.
Keywords: behavior change; foodborne illness; marketing; organizational culture; risk communication
 Of a dozen complaints in that period, there were four last year and only one this year.
Of a dozen complaints in that period, there were four last year and only one this year.
(1).jpg) However, it remains a challenge to compel food producers, processors, distributors, retailers, foodservice outlets and home meal preparers to adopt scientifically validated safe food handling behaviors, especially in the absence of an outbreak.
However, it remains a challenge to compel food producers, processors, distributors, retailers, foodservice outlets and home meal preparers to adopt scientifically validated safe food handling behaviors, especially in the absence of an outbreak. • stay up-to-date on emerging food safety issues;
• stay up-to-date on emerging food safety issues;.jpg) encouragement and enforcement to foster a food safety culture; and use technology to be transparent – whether it’s live webcams in the facility or real-time test results on the website – to help restore the shattered trust with the buying public.
encouragement and enforcement to foster a food safety culture; and use technology to be transparent – whether it’s live webcams in the facility or real-time test results on the website – to help restore the shattered trust with the buying public.(1)(1).jpg) demonstrable way. In an organization with a good food safety culture, individuals are expected to enact practices that represent the shared value system and point out where others may fail. By using a variety of tools, consequences and incentives, businesses can demonstrate to their staff and customers that they are aware of current food safety issues, that they can learn from others’ mistakes, and that food safety is important within the organization. The three case studies presented in this paper demonstrate that creating a culture of food safety requires application of the best science with the best management and communication systems, including compelling, rapid, relevant, reliable and repeated food safety messages using multiple media.
demonstrable way. In an organization with a good food safety culture, individuals are expected to enact practices that represent the shared value system and point out where others may fail. By using a variety of tools, consequences and incentives, businesses can demonstrate to their staff and customers that they are aware of current food safety issues, that they can learn from others’ mistakes, and that food safety is important within the organization. The three case studies presented in this paper demonstrate that creating a culture of food safety requires application of the best science with the best management and communication systems, including compelling, rapid, relevant, reliable and repeated food safety messages using multiple media. “Now that we are three years beyond that, it’s almost always hard to go back and put our mind where it was in 2005 and 2006 because we know so much more today than we knew then.”
“Now that we are three years beyond that, it’s almost always hard to go back and put our mind where it was in 2005 and 2006 because we know so much more today than we knew then.”