Cathy Owen of Wales Online writes a dad-of-three has been left paralysed after developing suspected food poisoning on a dream holiday to celebrate his 25th wedding anniversary.
 William Marsh, from Mountain Ash, was in a coma for 10 weeks and spent seven months in hospital after becoming ill on a holiday to the Dominican Republic with his wife Kathyrn two years ago.
William Marsh, from Mountain Ash, was in a coma for 10 weeks and spent seven months in hospital after becoming ill on a holiday to the Dominican Republic with his wife Kathyrn two years ago.
The 57-year-old has been diagnosed with the rare condition Guillain-Barré syndrome, a serious neurological condition which is a known complication from food poisoning.
He has now called on specialist serious injury lawyers to investigate his “devastating” ordeal.
William started suffering from stomach cramps and diarrhoea towards the end of a week-long all-inclusive at the Riu Naiboa resort which was booked to celebrate his 25th wedding anniversary.
When he got back home to Wales, the symptoms continued and on the day he was due to return to work as an engineer he woke up to find he had no feeling in his legs.
That sensation then started to spread across his entire body and William was diagnosed with Guillain-Barré syndrome.
William said: “Kathryn and my daughter fell ill first and then it hit me. The symptoms were awful but we just tried to push through it. I needed to get myself to work, so I thought nothing of it really.
“But then I got a huge shock when I woke up one morning and couldn’t feel my legs.”
William was on a ventilator in Prince Charles Hospital in Merthyr Tydfil and after a long period of treatment he was able to return home. But his life has now changed massively.
Almost two years on from his diagnosis, the father-of-three still cannot walk and is essentially confined to his living room due to the extent of his needs. He has been unable to return to work.
Guillain-Barré syndrome (GBS) is an autoimmune condition affecting the peripheral nervous system.
Often triggered by a viral or bacterial infection such as flu or food poisoning, it causes the nerves in the arms and legs to become inflamed and stop working, usually leading to temporary paralysis which may last from a few days to many months.
An estimated 1,300 people (one to two people per 100,000) are affected by GBS annually in the UK. About 80 per cent will make a good recovery, but between five and 10 per cent of people will not survive and 10-15 per cent may experience long term residual effects ranging from limited mobility or dexterity, to life-long dependency on a wheelchair.





 sample and stool samples that were submitted for testing.
sample and stool samples that were submitted for testing. .jpg)
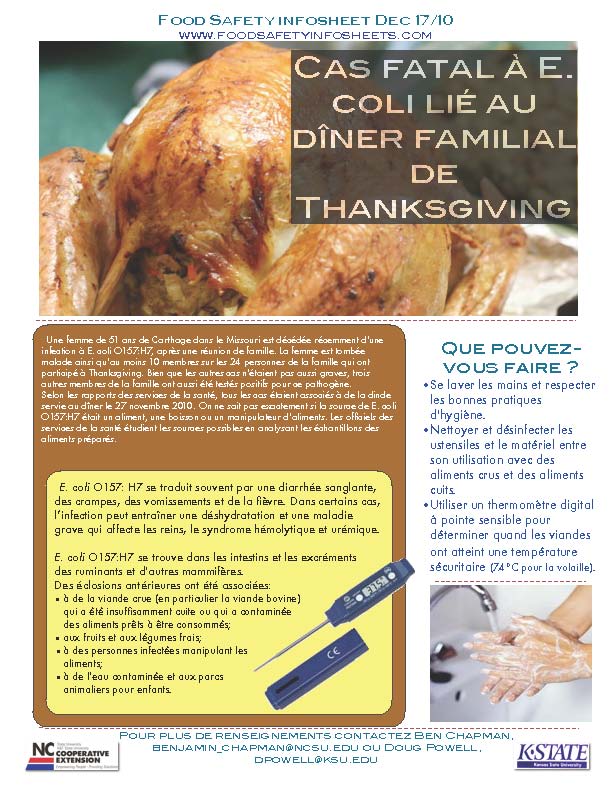 source de E. coli O157:H7 était un aliment, une boisson ou un manipulateur d’aliments. Les officiels des services de la santé étudient les sources possibles en analysant les échantillons des aliments préparés.
source de E. coli O157:H7 était un aliment, une boisson ou un manipulateur d’aliments. Les officiels des services de la santé étudient les sources possibles en analysant les échantillons des aliments préparés..jpg) today, with nary a mention of thermometers.
today, with nary a mention of thermometers. lavadero, y contaminar alimentos listos para comer que estén a dicha distancia.
lavadero, y contaminar alimentos listos para comer que estén a dicha distancia.