The U.S. Centers for Disease Control reports this outbreak investigation is over. Illnesses could continue because people may not know they could get a Salmonella infection from contact with dairy calves or other cattle.
 CDC, several states, and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) investigated a multistate outbreak of multidrug-resistant Salmonella Heidelberg infections. Epidemiologic and laboratory evidence indicated that contact with dairy calves and other cattle was the likely source of this outbreak.
CDC, several states, and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) investigated a multistate outbreak of multidrug-resistant Salmonella Heidelberg infections. Epidemiologic and laboratory evidence indicated that contact with dairy calves and other cattle was the likely source of this outbreak.
A total of 56 people infected with the outbreak strains of Salmonella Heidelberg were reported from 15 states. Illnesses started on dates ranging from January 27, 2015 to November 25, 2017. Of those with available information:
35% of people were hospitalized. No deaths were reported.
35% of people in this outbreak are children younger than 5 years.
Epidemiologic, laboratory, and traceback investigations linked ill people in this outbreak to contact with calves, including dairy calves.
In interviews, ill people answered questions about contact with animals and foods eaten in the week before becoming ill. Of the 54 people interviewed, 34 (63%) reported contact with dairy calves or other cattle. Some of the ill people interviewed reported that they became sick after their calves became sick or died.
Surveillance in veterinary diagnostic laboratories showed that calves in several states were infected with the outbreak strains of multidrug-resistant Salmonella Heidelberg
Information collected earlier in the outbreak indicated that most of the calves came from Wisconsin. Regulatory officials in several states attempted to trace the origin of calves linked to more recent illnesses. A specific source of cattle linked to newer illnesses was not identified.
Antibiotic resistance testing conducted by CDC on clinical isolates from ill people shows that the isolates were resistant to multiple antibiotics.
Antibiotic resistance may be associated with increased risk of hospitalization, development of a bloodstream infection, or treatment failure in patients.
Whole genome sequencing analysis identified predicted antibiotic resistance in outbreak-associated isolates from 48 ill people, in 88 isolates from cattle, and in 13 isolates from animal environments.
These findings match results from standard antibiotic resistance testing methods used by CDC’s National Antimicrobial Resistance Monitoring System (NARMS) laboratory on 10 isolates from 9 ill people and 1 animal. All 10 isolates were resistant to amoxicillin-clavulanic acid, ampicillin, cefoxitin, ceftriaxone, streptomycin, sulfisoxazole, and tetracycline. In addition, nine had reduced susceptibility to ciprofloxacin, nine were resistant to trimethoprim-sulfamethoxazole, six were resistant to nalidixic acid, four were resistant to chloramphenicol, and one was resistant to gentamicin. All 10 isolates tested were susceptible to azithromycin and meropenem.
Follow these steps to prevent illness when working with any livestock:
Always wash your hands thoroughly with soap and water right after touching livestock, equipment, or anything in the area where animals live and roam. Use dedicated clothes, shoes, and work gloves when working with livestock. Keep and store these items outside of your home.
It is especially important to follow these steps if there are children younger than 5 years in your household. Young children are more likely to get a Salmonella infection because their immune systems are still developing.
Work with your veterinarian to keep your animals healthy and prevent diseases.
It is important to remember that cattle can carry Salmonella and not appear sick. However, in this outbreak, some people did notice illness in their cattle, especially among calves. Livestock handlers should watch for sicknesses in dairy calves and consult their veterinarian if needed.




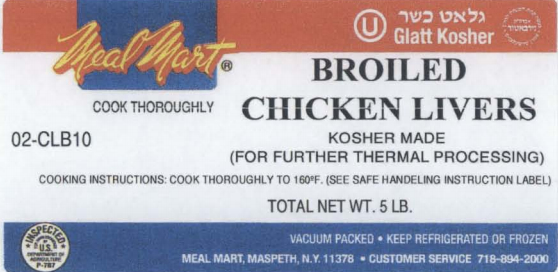 • Contaminated "kosher broiled chicken livers" were recalled from grocery stores but may still be in consumers’ homes.
• Contaminated "kosher broiled chicken livers" were recalled from grocery stores but may still be in consumers’ homes. products and an estimated 77 illnesses reported in 26 states. The illnesses were linked through an epidemiologic investigation and PFGE analyses by state health departments and The Centers for Disease Control and Prevention (CDC).
products and an estimated 77 illnesses reported in 26 states. The illnesses were linked through an epidemiologic investigation and PFGE analyses by state health departments and The Centers for Disease Control and Prevention (CDC).