Today (yesterday), World Hand Hygiene Day, the U.S. Centers for Disease Control is launching the new “Clean Hands Count” campaign urging healthcare professionals, patients, and patients’ loved ones to prevent healthcare-associated infections by keeping their hands clean.
 Although hand contact is known to be a major way germs spread in medical facilities, studies show that some healthcare professionals don’t follow CDC hand hygiene recommendations. On average, healthcare professionals clean their hands less than half of the times they should.
Although hand contact is known to be a major way germs spread in medical facilities, studies show that some healthcare professionals don’t follow CDC hand hygiene recommendations. On average, healthcare professionals clean their hands less than half of the times they should.
“Patients depend on their medical team to help them get well, and the first step is making sure healthcare professionals aren’t exposing them to new infections,” said CDC Director Tom Frieden, M.D., M.P.H. “Clean hands really do count and in some cases can be a matter of life and death.”
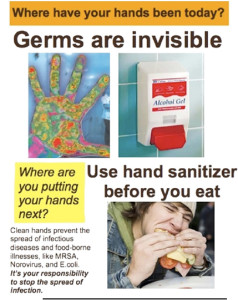
Part of the new campaign promotes healthcare provider adherence to CDC hand hygiene recommendations by addressing some of the myths and misperceptions about hand hygiene. For example, some people wrongly believe that using alcohol-based hand sanitizer contributes to antibiotic resistance and that it is more damaging to hands than washing with soap and water. Alcohol-based hand sanitizer kills germs quickly and in a different way than antibiotics, so it does not cause antibiotic resistance, and it causes less skin irritation than frequent use of soap and water.
The initiative also encourages patients and their loved ones to ask their healthcare team to clean their hands if they don’t see them do so before providing care.
“We know that patients can feel hesitant to speak up, but they are important members of the health care team and should expect clean hands from providers,” said Arjun Srinivasan, M.D., CDC’s associate director for healthcare-associated infection prevention programs. “We know that healthcare providers want the best for their patients, so we want to remind them that the simple step of cleaning their hands protects their patients.”
That’s right, it’s up to the dying and preoccupied family to ensure medical types wash their damn hands.
visit: www.cdc.gov/handhygiene.