Sorenne rode her bike to school on Friday for the first time.
After months of angst, probably because she saw daddy wipe out and get 23 stiches a couple of years ago when she was on training wheels, she rode her bike.
Today (Wed) they had a bike-to-school day to play-bicycle-polo-on-the-tennis courts, and the number of kids and bikes was a bit much to handle.
But that’s a good problem.
 I was chatting with a parent after school, while the kids retrieved their bikes that were stored at the swimming pool due to overload, and I said it was a nice problem to have, and then we chatted about the weather – depths of winter, 24C in Brisbane – and he said I guess spring has sprung, our backyard chickens laid two eggs yesterday, so I guess spring is here.
I was chatting with a parent after school, while the kids retrieved their bikes that were stored at the swimming pool due to overload, and I said it was a nice problem to have, and then we chatted about the weather – depths of winter, 24C in Brisbane – and he said I guess spring has sprung, our backyard chickens laid two eggs yesterday, so I guess spring is here.
I smiled but inside I was doing my best Jean-Luc.
The U.S. Centers for Disease Control and Prevention reports there are now eight multistate outbreaks of human Salmonella infections linked to contact with live poultry in backyard flocks.
In the eight outbreaks, 611 people infected with the outbreak strains of Salmonella were reported from 45 states.
Illnesses started on dates ranging from January 4, 2016 to June 25, 2016.
138 ill people were hospitalized, and one death was reported. Salmonella infection was not considered to be a cause of death.
195 (32%) ill people were children 5 years of age or younger.
Epidemiologic, traceback, and laboratory findings have linked the eight outbreaks to contact with live poultry such as chicks and ducklings sourced from multiple hatcheries.
Regardless of where they were purchased, all live poultry can carry Salmonella bacteria, even if they look healthy and clean.
These outbreaks are a reminder to follow steps to enjoy your backyard flock and keep your family healthy.
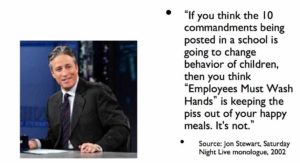
Always wash hands thoroughly with soap and water right after touching live poultry or anything in the area where the birds live and roam.
 Do not let live poultry inside the house.
Do not let live poultry inside the house.
Do not let children younger than 5 years of age handle or touch chicks, ducklings, or other live poultry without adult supervision.
These outbreaks are expected to continue for the next several months since flock owners might be unaware of the risk of Salmonella infection from live poultry or participate in risky behaviors that can result in infection.
Ill people reported purchasing live baby poultry from several suppliers, including feed supply stores, Internet sites, hatcheries, and friends in multiple states. Ill people reported purchasing live poultry to produce eggs, learn about agriculture, have as a hobby, enjoy for fun, keep as pets, or to give as Easter gifts. Some of the places ill people reported contact with live poultry include their home, someone else’s home, work, or school settings.
Public health officials collected samples from live poultry and the environments where the poultry live and roam from the homes of ill people in several states. Laboratory testing isolated four of the outbreak strains of Salmonella.
 KState has changed its handwashing recommendations.
KState has changed its handwashing recommendations.