Hand hygiene rates were found to be three times higher when auditors were visible to healthcare workers than when there were no auditors present, according to a study in a major Canadian acute care hospital.
 The study, titled, “Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study,” published today on-line in the BMJ Quality & Safety Journal, by first author Dr. Jocelyn Srigley, who did the study as part of her Master’s thesis while a Clinical Fellow in Infection Prevention and Control at University Health Network and University of Toronto and senior author Dr. Michael Gardam, Director, Infection Prevention and Control, University Health Network and Women’s College Hospital. Link: http://qualitysafety.bmj.com/cgi/rapidpdf/bmjqs-2014-003080?ijkey=JPbRe7gYzAFsm1Z&keytype=ref
The study, titled, “Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study,” published today on-line in the BMJ Quality & Safety Journal, by first author Dr. Jocelyn Srigley, who did the study as part of her Master’s thesis while a Clinical Fellow in Infection Prevention and Control at University Health Network and University of Toronto and senior author Dr. Michael Gardam, Director, Infection Prevention and Control, University Health Network and Women’s College Hospital. Link: http://qualitysafety.bmj.com/cgi/rapidpdf/bmjqs-2014-003080?ijkey=JPbRe7gYzAFsm1Z&keytype=ref
The study examined the Hawthorne effect, also known as observation bias – the tendency of people to change their behavior when they are aware of an observer – using an electronic monitoring hand hygiene system in real-time, eliminating many of the biases inherent to human observation. Ultrasound “tags” on soap dispensers transmitted a signal to a nearby receiver each time the levers were pushed, and a time-stamped hand hygiene wash was recorded in a central data base.
Two inpatient units in University Health Network were electronically monitored, with 60 healthcare workers volunteering to be part of a study of the electronic monitoring system. Staff were aware that data would be used in a variety of studies, but were “blind” to the questions asked in the studies. Auditors did not announce their presence during audits but wore white lab coats. Auditors were also blinded to the questions asked in the research. Hand hygiene dispenses were electronically measured while the auditors were visible, and were compared to the same locations prior to the arrival of the auditors at one, two and three weeks before the audit, as well as to a different area of the unit not visible to the auditor. Auditors typically did not go into patient rooms, so separate hand washing rates were determined for dispensers inside patient rooms and those in hallways. Twelve audits were included between November 2012 and March 2013.
 The study found that there was an approximately three-fold increase in the rate of hallway hand washes per hour amongst healthcare staff when an auditor was visible (3.75 per hour), compared to a location where the auditor was not visible (1.48 per hour) and to the previous weeks (1.07 per hour). Hand washing rates with the auditor present were compared to separate groups at different time periods and locations to ensure that the differences found were not due to hand hygiene patterns that could be attributable to time of day or location. In each instance, the hand washing rates were significantly higher when the auditors were present, with the increase occurring after the auditors’ arrival, suggesting that the arrival of the auditor triggered the increase in hand hygiene.
The study found that there was an approximately three-fold increase in the rate of hallway hand washes per hour amongst healthcare staff when an auditor was visible (3.75 per hour), compared to a location where the auditor was not visible (1.48 per hour) and to the previous weeks (1.07 per hour). Hand washing rates with the auditor present were compared to separate groups at different time periods and locations to ensure that the differences found were not due to hand hygiene patterns that could be attributable to time of day or location. In each instance, the hand washing rates were significantly higher when the auditors were present, with the increase occurring after the auditors’ arrival, suggesting that the arrival of the auditor triggered the increase in hand hygiene.
“The difference in hand hygiene rates, when an auditor is present compared to those times when one is not, is huge in this study, and we showed this effect to be very consistent,” says Dr. Gardam, who is also an Associate Professor of Medicine at the University of Toronto.
“The magnitude of what we found calls into question the accuracy of directly observed hand hygiene rates and the usefulness of measuring and reporting them,” says Dr. Gardam. “That said, human auditing of hand hygiene has been helpful to draw attention to this important preventative measure—we just can’t stop focusing on it because our posted rates are not nearly as high as we think they are.”
Dr. Srigley says that although the researchers were “surprised at the tripling effect” of having an auditor present, there may still be some value in doing audits as there could be opportunities for in-the-moment education with health care staff. Dr. Srigley is the Associate Medical Director of Infection Prevention and Control at Hamilton Health Sciences, composed of seven hospitals in the Hamilton area.
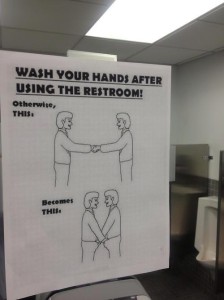
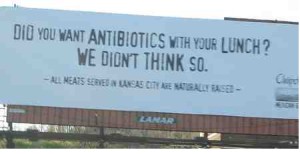
Dr. Gardam suggests that a “front-line staff ownership” approach which engages rather than “nags” staff is a good option. This approach was first brought to University Health Network about six years by Dr. Gardam, in which front-line staff have developed their own reminders to influence staff to wash their hands, including: pancake breakfasts, public unit reporting, pledges, posters, and holding each other accountable.
“We need to change how we look at these complex problems,” says Dr. Gardam, “We need to help people change by engaging them and having them come up with local solutions.”
 The restaurant, located at 860 Macon Highway in Lawrenceville, scored 60 out of 100.
The restaurant, located at 860 Macon Highway in Lawrenceville, scored 60 out of 100.