My friend and hockey goon Kevin Allen at the University of British Columbia makes some good points about policy after one person died and 16 others were sickened with E. coli O157:H7 via raw 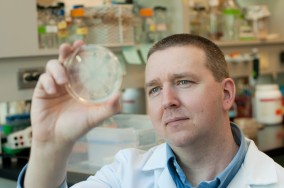 milk cheese in Canada.
milk cheese in Canada.
Dr. Robert Parker, the chief medical officer for the B.C. Interior Health Authority, makes some lousy points about policy and when to go public.
According to CBC, health officials suspected an E. coli outbreak was linked to a B.C. cheese farm as early as last Friday, but waited until Tuesday to warn the public because they had to be certain of the source. The Canadian Food Inspection Agency confirmed one person has died and 10 people are ill from consuming raw milk cheese products from B.C. Gort’s Gouda has been linked to an outbreak of E. coli in B.C. and Alberta
Parker says media attention can destroy a business, and authorities wanted to be certain. He says people do not need to stop eating cheese made from raw milk, since there have not been several outbreaks. “I think if we start seeing repeated outbreaks in unpasteurized cheese products, it might be worthwhile to review again,” said Parker.
There have been endless and a disproportionately high number of outbreaks associated with raw milk cheese. Parker should know that.
Publicly available guidelines for when to go public with health information that are consistently followed by health types, would  remove many conspiratorial elements.
remove many conspiratorial elements.
Edmonton’s Annemarie McCrie ate at Gort’s Farm on Sept. 1 on her way back home from vacation in B.C. with a friend. “We wanted to stop and there’s a little sign that said ‘cheese farm’ – so I thought ‘oh, let’s go to the cheese farm,’ because everybody wants to visit a cheese farm.”
I don’t.
Kevin Allen, a University of British Columbia microbiologist, says this recall highlights the problems associated with consuming raw milk and its products. “Obviously we have a failure here,” says Allen. Allen says currently Canadian law requires raw milk cheese to be aged for 60 days in order to eliminate pathogens and make it safe, but E. coli O157 can survive well past that time and aging is not a guarantee of safety. “The problem is we have a modern-day food chain with modern-day pathogens that seem tolerant to these  conditions that we use to render it safe,” says Allen. “I think it’s maybe time to look at our policy and maybe amend it.”
conditions that we use to render it safe,” says Allen. “I think it’s maybe time to look at our policy and maybe amend it.”
A Calgary cheesemaker whose family has been in the cheese business for roughly 300 years wants to see unpasteurized cheese banned in Canada.







 Saturday.
Saturday.