This study describes trends in the incidence of pregnancy-related listeriosis in France between 1984 and 2011, and presents the major characteristics of 606 cases reported between 1999 and 2011 to the French Institute for Public Health Surveillance through the mandatory notification system.
 The incidence of pregnancy-related listeriosis decreased by a factor of 12 from 1984 to 2011. This reduction was a result of progressive implementation of specific Listeria monocytogenes control measures in food production. A lower incidence of pregnancy-related listeriosis was observed in regions with a lower prevalence of toxoplasmosis. Given that dietary recommendations in pregnancy target both toxoplasmosis and listeriosis prevention, we suppose that recommendations may have been delivered and followed more frequently in these regions.
The incidence of pregnancy-related listeriosis decreased by a factor of 12 from 1984 to 2011. This reduction was a result of progressive implementation of specific Listeria monocytogenes control measures in food production. A lower incidence of pregnancy-related listeriosis was observed in regions with a lower prevalence of toxoplasmosis. Given that dietary recommendations in pregnancy target both toxoplasmosis and listeriosis prevention, we suppose that recommendations may have been delivered and followed more frequently in these regions.
Cases reported between 1999 and 2011 (n=606) were classified as maternal infections with ongoing pregnancy (n=89, 15%), fetal loss (n=166, 27%), or live-born neonatal listeriosis (n=351, 58%). The majority of live-born neonatal listeriosis cases (n=216, 64%) were preterm births (22–36 weeks of gestation), of whom 14% (n=30) were extremely preterm births (22–27 weeks of gestation). Eighty per cent of mothers reported having eaten high risk food during pregnancy. A better awareness of dietary recommendations in pregnant women is therefore necessary.
Eurosurveillance, Volume 19, Issue 38
D Girard, A Leclercq, E Laurent, M Lecuit, H de Valk, V Goulet
http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20909
Listeriosis, caused by Listeria monocytogenes, is an important foodborne disease that can be difficult to control and commonly results in severe clinical outcomes. We aimed to provide the first estimates of global numbers of illnesses, deaths, and disability-adjusted life-years (DALYs) due to listeriosis, by synthesising information and knowledge through a systematic review.
Methods
We retrieved data on listeriosis through a systematic review of peer-reviewed and grey literature (published in 1990—2012). We excluded incidence data from before 1990 from the analysis. We reviewed national surveillance data where available. We did a multilevel meta-analysis to impute missing country-specific listeriosis incidence rates. We used a meta-regression to calculate the proportions of health states, and a Monte Carlo simulation to generate DALYs by WHO subregion.
Findings
We screened 11 722 references and identified 87 eligible studies containing listeriosis data for inclusion in the meta-analyses. We estimated that, in 2010, listeriosis resulted in 23 150 illnesses (95% credible interval 6061—91 247), 5463 deaths (1401—21 497), and 172 823 DALYs (44 079—676 465). The proportion of perinatal cases was 20·7% (SD 1·7).
Interpretation
Our quantification of the global burden of listeriosis will enable international prioritisation exercises. The number of DALYs due to listeriosis was lower than those due to congenital toxoplasmosis but accords with those due to echinococcosis. Urgent efforts are needed to fill the missing data in developing countries. We were unable to identify incidence data for the AFRO, EMRO, and SEARO WHO regions.
Funding
WHO Foodborne Diseases Epidemiology Reference Group and the Université catholique de Louvain.
The Lancet Infectious Diseases, doi:10.1016/S1473-3099(14)70870-9
Noordhout, Charline Maertens De, Brecht Devleesschauwer, Frederick J. Angulo, Geert Verbeke, Juanita Haagsma, Martyn Kirk, Arie Havelaar, and Niko Speybroeck
http://www.thelancet.com/journals/laninf/article/PIIS1473-3099(14)70870-9/abstract
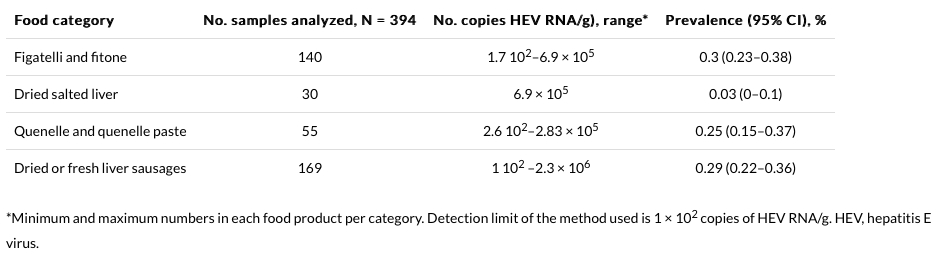
 Acute autochthonous HE cases confirmed by the National Reference Centre (CNR) were interviewed on exposures in the 2 to 10 weeks before illness onset. Clinical, biological and epidemiological characteristics were documented for 139 autochthonous cases.
Acute autochthonous HE cases confirmed by the National Reference Centre (CNR) were interviewed on exposures in the 2 to 10 weeks before illness onset. Clinical, biological and epidemiological characteristics were documented for 139 autochthonous cases.