Maple Leaf Foods president and CEO Michael McCain said last night that “consistent with normal findings and practices” listeria continues to be found at the same facility that produced cold-cuts linked to at least 20 deaths and 50 illnesses in Canada.
“Listeriosis is an exceptionally rare illness,” he said, “but we are taking every precaution possible.”
(1).jpg) I’m sure the illness didn’t feel exceptionally rare to the sick and the dead.
I’m sure the illness didn’t feel exceptionally rare to the sick and the dead.
Mr. McCain also reiterated that,
“Listeria exists in all food plants, all supermarkets and presumably in all kitchens,”
which is exactly why my pregnant wife and Ben’s pregnant wife didn’t go near Maple Leaf or any other cold cuts during their pregnancies. So I’m sure Mr. McCain will put as much energy and resources into advising vulnerable populations to stay away from Maple Leaf cold-cuts and other refrigerated ready-to-eat foods as he is into re-opening the Toronto plant.
And if Maple Leaf is now “behaving in the most conservative way possible,” what were they doing before the listeria outbreak became public knowledge on Aug. 20, 2008?
Confidential data obtained by the Toronto Star and CBC and reported last night revealed that two-thirds of Maple Leaf meat samples collected from Toronto hospitals and nursing homes tested positive for a virulent strain of listeria just before the country’s largest food recall.
The test results show a dramatically high percentage of bacteria-laced ham, corned beef, turkey, and roast beef was being served to hundreds of vulnerable hospital patients and seniors. Experts say it’s more contamination than they have seen and further evidence of a health risk that should have reached the public’s attention sooner.
“There shouldn’t be any positives,” says Rick Holley, a food safety expert at the University of Manitoba. “The reality is if you did a survey in the market, you might find one or two at most out of this sample that are positive … And it is a particularly virulent strain of listeria. It’s one of the bad ones.” …
“I’d never seen anything like this,” said Dr. Vinita Dubey, Toronto’s associate medical officer of health. “The fact that so many came back positive shows how contaminated the source was.”
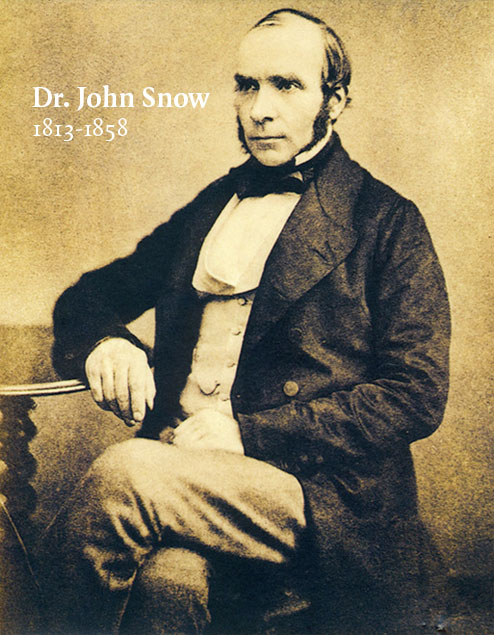
(2).gif) So given the high level of contamination, what did the Canadian Food Inspection Agency do? Insist on more testing, because epidemiology is not enough to protect the health of Canadians.
So given the high level of contamination, what did the Canadian Food Inspection Agency do? Insist on more testing, because epidemiology is not enough to protect the health of Canadians.
In a conference call with members of the Canadian Food Inspection Agency on Aug. 14, Toronto officials told the agency they had enough evidence to make a connection and pressed the CFIA to warn the public about Maple Leaf products.
CFIA officials, however, said they needed to wait for one more set of test results from unopened meat packages.
While the CFIA had identified listeria bacteria at the Maple Leaf Foods meat processing plant in Toronto and even begun an investigation of the company by that time, the federal agency said it wanted definitive test results to see whether it was the same strain as the one responsible for the outbreak.
The CFIA declined a request for an interview with CBC News. The agency maintained that it requires hard scientific proof before it can recall food or issue warnings to the public.
Toronto Public Health said it had gathered plenty of evidence during July and August that linked Maple Leaf meat products to the outbreak, including:
* two deaths linked to listeriosis
* more cases being reported
* meat samples from sandwiches tested positive
* samples from opened meat packages were taken
During a 2005 outbreak of salmonella found in bean sprouts in Kingston, Ont., regional health officials didn’t wait for definitive proof to issue their own recall.
 "I think it’s a less desirable approach, from the point of view of the people we serve, to say, ‘We’ll have to wait and have confirmation before we can intervene,’" said Dr. Ian Gemmill, the medical officer of health for the Kingston Area Health Unit.
"I think it’s a less desirable approach, from the point of view of the people we serve, to say, ‘We’ll have to wait and have confirmation before we can intervene,’" said Dr. Ian Gemmill, the medical officer of health for the Kingston Area Health Unit.
The locals sound increasingly frustrated with CFIA. Until there is a clear policy on when to go public, expect more failures and frustration in the future.
Asked for the listeria test results leading up to the outbreak, the Maple Leaf spokesthingy said last week that, in the spirit of open and transparent co-operation and a genuine desire to improve the safety of refrigerated, ready-to-eat foods, the company would not release them publicly.
 hanging out with the goddess of porcelain.
hanging out with the goddess of porcelain. But not so concerned to issue a warning earlier. Who knew what when? Maybe it’s time to pull back the curtain on epidemiological investigations and when to go public with information that could prevent others from barfing.
But not so concerned to issue a warning earlier. Who knew what when? Maybe it’s time to pull back the curtain on epidemiological investigations and when to go public with information that could prevent others from barfing.
 The guidelines in this document are targeted to local, state and federal agencies and provide model practices used in foodborne disease outbreaks, including planning, detection, investigation, control and prevention. Local and state agencies vary in their approach to, experience with, and capacity to respond to foodborne disease outbreaks. The guidelines are intended to give all agencies a common foundation from which to work and to provide examples of the key activities that should occur during the response to outbreaks of foodborne disease. The guidelines were developed by a broad range of contributors from local, state and federal agencies with expertise in epidemiology, environmental health, laboratory science and communications. The document has gone through a public review and comment process.
The guidelines in this document are targeted to local, state and federal agencies and provide model practices used in foodborne disease outbreaks, including planning, detection, investigation, control and prevention. Local and state agencies vary in their approach to, experience with, and capacity to respond to foodborne disease outbreaks. The guidelines are intended to give all agencies a common foundation from which to work and to provide examples of the key activities that should occur during the response to outbreaks of foodborne disease. The guidelines were developed by a broad range of contributors from local, state and federal agencies with expertise in epidemiology, environmental health, laboratory science and communications. The document has gone through a public review and comment process. The idea food that is grown and consumed locally is somehow safer than other food, either because it contacts fewer hands or any outbreaks would be contained, is sorta soothing, like a mild hallucinogen, and has absolutely no basis in reality.
The idea food that is grown and consumed locally is somehow safer than other food, either because it contacts fewer hands or any outbreaks would be contained, is sorta soothing, like a mild hallucinogen, and has absolutely no basis in reality..jpg) But the absence of data doesn’t stop doctrine. JoLynn Montgomery, director of the Michigan Center for Public Health Preparedness at the University of Michigan told the
But the absence of data doesn’t stop doctrine. JoLynn Montgomery, director of the Michigan Center for Public Health Preparedness at the University of Michigan told the  Locust Grove, Oklahoma, was also hammered by an E. coli outbreak, E. coli O111, linked to dining at the Country Cottage restaurant in August.. One person died, 72 were hospitalized and 241 others got sick before the outbreak was contained.
Locust Grove, Oklahoma, was also hammered by an E. coli outbreak, E. coli O111, linked to dining at the Country Cottage restaurant in August.. One person died, 72 were hospitalized and 241 others got sick before the outbreak was contained.(1).jpg) I’m sure the illness didn’t feel exceptionally rare to the sick and the dead.
I’m sure the illness didn’t feel exceptionally rare to the sick and the dead.(2).gif) So given the high level of contamination, what did the Canadian Food Inspection Agency do? Insist on more testing, because
So given the high level of contamination, what did the Canadian Food Inspection Agency do? Insist on more testing, because  "I think it’s a less desirable approach, from the point of view of the people we serve, to say, ‘We’ll have to wait and have confirmation before we can intervene,’" said Dr. Ian Gemmill, the medical officer of health for the Kingston Area Health Unit.
"I think it’s a less desirable approach, from the point of view of the people we serve, to say, ‘We’ll have to wait and have confirmation before we can intervene,’" said Dr. Ian Gemmill, the medical officer of health for the Kingston Area Health Unit. The president of Honduras is furious. So is the agriculture minister who is demanding millions in reparations, saying the U.S. has not scientifically proven the fruit was infected in Honduras.
The president of Honduras is furious. So is the agriculture minister who is demanding millions in reparations, saying the U.S. has not scientifically proven the fruit was infected in Honduras..jpg) It’s often not fair. Any hosehead can come along and say, "Hey, I found a mouse in my beer bottle, give me a free case of beer." Or a syringe in some soda. Or I barfed from eating some food. The best producers or manufacturers can do is diligently manage and mitigate risks and be able to prove such diligence in the court of public opinion.
It’s often not fair. Any hosehead can come along and say, "Hey, I found a mouse in my beer bottle, give me a free case of beer." Or a syringe in some soda. Or I barfed from eating some food. The best producers or manufacturers can do is diligently manage and mitigate risks and be able to prove such diligence in the court of public opinion.