I’m always wondering about the microbiological loads on aprons those food porn chefs wear on TV; or in their kitchens; or wherever else their food fantasies take them.
Someone else decided to take a look at the loads on those white lab-style coats doctors wear.
Some have feared that long-sleeved coats and other garments can spread MRSA and other nasty bacteria around the workplace, but a newly published randomized trial finds there’s no added risk.
The study, published in the Journal of Hospital Medicine, was conducted by researchers from the University of Colorado. They randomly assigned 100 medical residents and hospitalists to wear either their own white coats or the kind of just-washed short-sleeve uniform thought to better prevent bacterial spread.
At eight hours into the work day, researchers took samples from breast pocket, sleeve cuff and skin of the wrist, then let them incubate. They found “no significant differences” between the bacterial colony counts from the coats and the uniforms — not on the sleeves (whether short or long) or pockets.
There was also no difference between the groups in the number of people carrying around the MRSA bacteria on their clothes or wrists.
No word on whether this will let physicians in the U.K. cover up again; the National Health Service banned long sleeves a few years ago.
In Toronto, Dr. Allison McGeer, director of infection control at Mount Sinai Hospital, said she found the study’s results to be "interesting and useful."
"I think there’s a lot of controversy about the extent to which we should be investing resources in having clothes that are not contaminated when it’s pretty clear that it’s not the clothes that make that much difference," she said, adding that hand hygiene and a number of other practice issues are more important.
"I don’t think this is enough evidence to say lab coats are not a problem. At the same time, honestly, I’m not that worried about lab coats. Not at the top of my list."

 out of your ear, you don’t know where that finger’s been (or where it’s going).
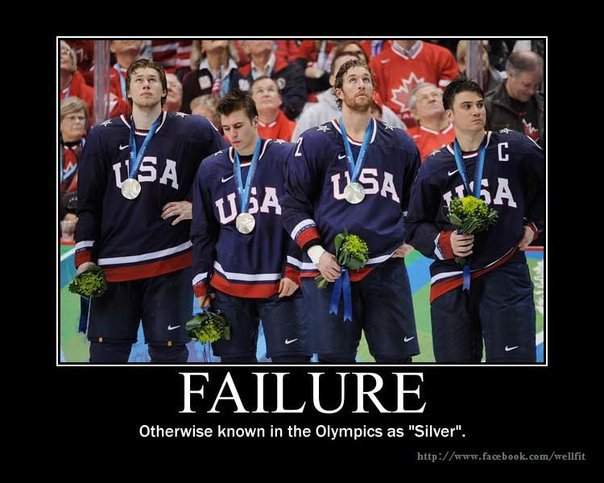
out of your ear, you don’t know where that finger’s been (or where it’s going)..jpg) Olympics? – and OK when the Canadian men won gold, but I still say Vancouver is a dump of a town. Always has been.
Olympics? – and OK when the Canadian men won gold, but I still say Vancouver is a dump of a town. Always has been.