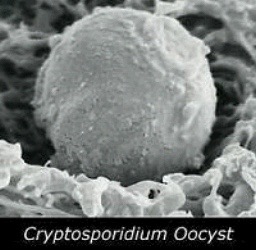
In May 2012, people in England and Scotland started getting sick with Cryptosporidium. In June, 2012, the UK Health Protection Agency first announced 267 people were sick with Cryptosporidium across four areas of the UK, double the normal rate.
 Ten months later, HPA said the crypto that sickened about 300 people was most likely linked to eating pre-cut bagged salad products which were likely to have been labeled as ‘ready-to-eat.’
Ten months later, HPA said the crypto that sickened about 300 people was most likely linked to eating pre-cut bagged salad products which were likely to have been labeled as ‘ready-to-eat.’
The outbreak was short lived and the numbers of cases returned to expected seasonal levels within a month of the first cases being reported. Most of those affected had a mild to moderate form of illness and there were no deaths associated with the outbreak.
During the investigation, an initial link was found between illness and pre-cut spinach. When specific retailers were included in the analysis, the strongest association with infection was found to be with consumption of ready to eat pre-cut mixed salad leaves from a major supermarket chain.
In this analysis, exposure to pre-cut spinach only reached conventional levels of significance for one retailer – a second major supermarket chain. A link to spinach from a number of other retailers was also suggested but these were not statistically significant. Together these findings suggest that one or more types of salad vegetables could have been contaminated.
Dr Stephen Morton, regional director of the HPA’s Yorkshire and the Humber region and head of the multi-agency Outbreak Control Team, said, “Our findings suggest that eating mixed leaf bagged salad was the most likely cause of illness. It is however often difficult to identify the source of short lived outbreaks of this type as by the time that the outbreak can be investigated, the affected food and much of the microbiological evidence may no longer be available
Dr Alison Gleadle, director of food safety at the FSA, took the opportunity to further confuse consumers, stating, “We’d like to remind everyone of our usual advice to wash all fruits and vegetables, including salad, before you eat them, unless they are labeled ready-to-eat.”
 But wasn’t this outbreak linked to ready-to-eat salads? How is that advice of any use? Could have offered some details, like, additional washing of ready-to-eat products is largely ineffective. FSA is refocusing its efforts on farm management to limit such contamination, before it happens.
But wasn’t this outbreak linked to ready-to-eat salads? How is that advice of any use? Could have offered some details, like, additional washing of ready-to-eat products is largely ineffective. FSA is refocusing its efforts on farm management to limit such contamination, before it happens.
A spokesthingy from retailer Morrisons said, rather defensively, “Morrisons is not the source of this outbreak. We have received no complaints of illness and no Morrisons products have tested positive for Cryptosporidia.
“The HPA’s claim is based solely on statistics, not testing. The very same statistics also implicated products from other retailers that the HPA recognize as ‘implausible’.”
Why doesn’t Morrison’s say what they do to enhance the safety of products they sell rather than trash epidemiology?
In the scientific paper on the outbreak, McKerr et. al reported a widespread foodborne outbreak of Cryptosporidium parvum in England and Scotland in May 2012. Cases were more common in female adults, and had no history of foreign travel. Over 300 excess cases were identified during the period of the outbreak. Speciation and microbiological typing revealed the outbreak strain to be C. parvum gp60 subtype IIaA15G2R1.
METHODS: Hypothesis generation questionnaires were administered and an unmatched case control study was undertaken to test the hypotheses raised. Cases and controls were interviewed by telephone. Controls were selected using sequential digit dialling. Information was gathered on demographics, foods consumed and retailers where foods were purchased.
RESULTS: Seventy-four laboratory confirmed cases and 74 controls were included in analyses. Infection was found to be strongly associated with the consumption of pre-cut mixed salad leaves sold by a single retailer. This is the largest documented outbreak of cryptosporidiosis attributed to a food vehicle.
An outbreak of cryptosporidium parvum across England & Scotland associated with consumption of fresh pre-cut salad leaves, May 2012
PubMed
McKerr C1, Adak GK2, Nichols G3, Gorton R4, Chalmers RM5, Kafatos
PLoS One, 2015, doi: 10.1371/journal.pone.0125955. eCollection 2015.
http://www.ncbi.nlm.nih.gov/m/pubmed/26017538/
 The Cochran–Armitage test was used to assess changes in the proportions of cases by case status (confirmed vs. non-confirmed), sex, race, and ethnicity over the study period. Negative binomial regression models were used to estimate rate ratios (RR) and 95% confidence intervals (CI) for comparing rates across three time periods (1995–2004, 2005–2008, 2009–2012). The proportion of confirmed cases significantly decreased (P < 0·0001), and a crossover from male to female predominance in case-patients occurred (P < 0·0001). Overall, compared to 1995–2004, rates were higher in 2005–2008 (RR 2·92, 95% CI 2·08–4·09) and 2009–2012 (RR 2·66, 95% CI 1·90–3·73). However, rate changes from 2005–2008 to 2009–2012 varied by age group (Pinteraction < 0·0001): 0–14 years (RR 0·55, 95% CI 0·42–0·71), 15–44 years (RR 0·99, 95% CI 0·82–1·19), 45–64 years (RR 1·47, 95% CI 1·21–1·79) and ≥65 years (RR 2·18, 95% CI 1·46–3·25).
The Cochran–Armitage test was used to assess changes in the proportions of cases by case status (confirmed vs. non-confirmed), sex, race, and ethnicity over the study period. Negative binomial regression models were used to estimate rate ratios (RR) and 95% confidence intervals (CI) for comparing rates across three time periods (1995–2004, 2005–2008, 2009–2012). The proportion of confirmed cases significantly decreased (P < 0·0001), and a crossover from male to female predominance in case-patients occurred (P < 0·0001). Overall, compared to 1995–2004, rates were higher in 2005–2008 (RR 2·92, 95% CI 2·08–4·09) and 2009–2012 (RR 2·66, 95% CI 1·90–3·73). However, rate changes from 2005–2008 to 2009–2012 varied by age group (Pinteraction < 0·0001): 0–14 years (RR 0·55, 95% CI 0·42–0·71), 15–44 years (RR 0·99, 95% CI 0·82–1·19), 45–64 years (RR 1·47, 95% CI 1·21–1·79) and ≥65 years (RR 2·18, 95% CI 1·46–3·25).