Mrs. Kalisz, my grade 7 and 8 family studies teacher warned of the dangers of botulism by showing our class a bulging can of beans (which she kept in a ziplock bag). What I took away from that story was to never buy or use dented cans (although that practice can be debated). Botulism from commercially canned foods has been pretty rare in North America since the 1970s with only a couple of cases in 40+ years.
The first case of food-related botulism recorded in the medical literature occurred in Germany in 1735 and was traced to uncooked fermented blood sausage. Food safety history guru (and pretty decent margarita recipe developer) Carl Custer pointed out in an IAFP workshop that botulism concerns (and regulatory responses) go back further than that. In the 10th century, Emperor Leo VI of Byzantium prohibited the manufacture of blood sausage because of repeated illnesses leaving folks paralyzed and dying not too long after exposure. Botulism (derived from botulus, the latin word for sausage) is pretty nasty.
In 2002, a Meaford, Ontario man fell ill with botulism after eating a toxin-containing baked potato from a local restaurant. A 35-year old father of two was still on life support two months later. Potatoes wrapped in tinfoil, baked, and then held at room temperature can create the perfect conditions for Clostridium botulinum problems.
The spores, found fairly commonly in soil, germinate and outgrow in anaerobic conditions (like partially-fermented sausages, under processed canned food, seafood and foil-wrapped baked potatoes) resulting in vegetative cells. A byproduct of the cells’ multiplication is the toxin.
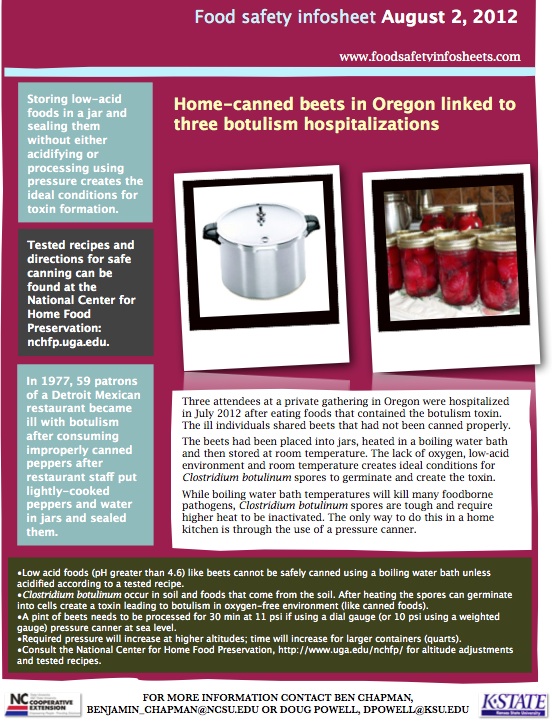
Although the memorable outbreaks are linked to commercial food, the most common source of botulism in North America is improperly canned home preserves, usually from low acid foods being placed into a jar and then heating enough to seal – but not enough to inactivate the C. botulinum spores. A few weeks ago Doug asked me for a recipe for acidified pickled onions which he wanted to keep refrigerated to control pathogen growth instead of messing with processing (right, exactly as shown). In 2012, a few unlucky folks attending a Oregon family gathering ate some beets that had been boiling-water-bathed, reaching just 212F instead of the needed 240F.
According to Diario Uno, 69 year-old Argentinean man died of botulism on March 10, 2013 after reportedly consuming home canned foods,
The man arrived at the hospital on Wed 6 Mar 2013, with acute pain; his condition deteriorated and he was admitted in the intensive care unit, where he died on Sun 10 Mar 2013. During the time of admission”different doctors treated him and carried out all possible diagnostic tests, arriving at a diagnosis of botulism for which the patient received treatment.” Dr Pedro Farran said, “Home canning is very common in our area; the problem is not in the food preparation but in its improper canning. Even marinades with low content of vinegar can transmit the disease.”





 contaminated with Clostridium botulinum.
contaminated with Clostridium botulinum.
 basketball-sized court surrounded by 20 feet of brick and topped with razor wire. People on the outside would flick half a cigarette, with the tobacco removed and filled with hashish, over the wall so it looked like another discarded butt.
basketball-sized court surrounded by 20 feet of brick and topped with razor wire. People on the outside would flick half a cigarette, with the tobacco removed and filled with hashish, over the wall so it looked like another discarded butt.