Ron Doering, former president of the Canadian Food Inspection Agency and current counsel in the Ottawa offices of Gowlings (Ronald.doering@gowlings.com), reports with part II of his take on antimicrobiasl in food animal production:
While the medical community recognizes that the emergence and spread of antimicrobial resistance (AMR) in humans is a potential disaster for humanity and that it is the overuse of antimicrobials in human medicine that is the largest contributor, there is a broad consensus that the use of antibiotics in animals contributes to the problem, though the scale is still unclear. This uncertainty is due mainly to a failure to adequately control and monitor the use. Health Canada (HC) lacks the authority to control and monitor use because the practice of veterinary medicine falls under provincial jurisdiction. Recognizing that almost all practical efforts to reduce the level of antibiotics in meat depend on the more active participation of veterinarians, HC announced recently that it wanted “to develop options to strengthen the veterinary oversight of antimicrobial use in food animals.”
 What can veterinarians and their provincial regulatory licensing bodies do now to reduce the threat of AMR? Here are four suggestions:
What can veterinarians and their provincial regulatory licensing bodies do now to reduce the threat of AMR? Here are four suggestions:
1. Enhance awareness among members .
While the Canadian Veterinary Medical Association (CVMA) has developed voluntary Prudent Use Guidelines, I’m told that many vets are hardly aware of the issue and may not even know of the Guidelines. Concerned enough about this, Ontario’s regulatory body, the College of Veterinarians of Ontario, just announced that it was launching a project to study the use of antibiotics among food animal veterinarians and to determine if they use the CVMA’s Guidelines in daily practice. Quebec requires a mandatory day-long AMR program and a test. All provinces should follow Quebec and develop mandatory continuing education programs on antimicrobial stewardship.
2. Fill the regulatory gaps.
As long as vets continue to prescribe off label use and the use of Active Pharmaceutical Ingredients (APIs) in production medicine, it’s impossible to know the level of antibiotic use. Own Use Importation (OUI) by animal owners is another avenue for which use information is unavailable. As one recent report stressed: “The gap in reliable usage data makes it difficult to state with confidence which antimicrobials are used, in what quantities, and for what purposes.” The recent critical assessment by a group of experts, titled “Stewardship of antimicrobial drugs in animals in Canada: How are we doing in 2013?” (Canadian Veterinary Journal, March 2014), highlighted the absolute importance of improving Canada’s monitoring of antimicrobial usage.
3. Conflict of interest issue.
This issue has been flagged by several reports going back to the landmark McEwen Report of 2002. Veterinarians obtain income from the profitable sale of antimicrobials. Decoupling veterinary prescribing from dispensing raises several issues because the current veterinary practice business model is based on an income stream from antimicrobial sales. Veterinarians should lead a dialogue on this important issue that clearly needs closer examination.
 4. Antibiotics for disease prevention.
4. Antibiotics for disease prevention.
The real issue is not the use of antibiotics for growth promotion or the treating of disease, but whether they should continue to be used for disease prevention. While some antibiotics of very high importance to human health should only be used to treat infection, there are several arguments that some of high or medium importance to human health (what HC calls Category ll and lll, for example tetracyclines) should still, with closer veterinarian oversight, be used for disease prevention. Because major retailers, processors and consumers increasingly demand meat with “raised without antibiotic” claims, the marketplace is forcing changes in practice. But we mustn’t lose sight of the fact that while there are risks to using antimicrobials in animal production, there are also risks with non-use.
Two-thirds of animal diseases are zoonotic, meaning the disease is transferable to humans. For this and other reasons, I have been a long-time proponent of strengthening the connections between human and animal medicine — the concept known as One Health. In this context, AMR represents an historic opportunity for vets to step up and provide greater leadership.




 best producers use techniques – regardless of political ideology – that fit best in their production system in their geographic location.
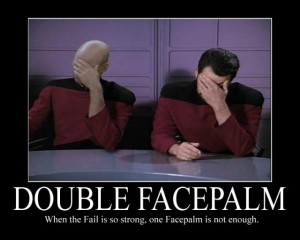
best producers use techniques – regardless of political ideology – that fit best in their production system in their geographic location. on the truly terrific television series, The Soprano’s (right).
on the truly terrific television series, The Soprano’s (right). Reminds me of that scene from
Reminds me of that scene from  Theo Weening, the national meat buyer for Whole Foods Market, says he “can assure our customers that our standard is: No antibiotics, EVER! We work very hard to make sure that the people who produce our meat have raised their animals without the use of antibiotics, growth hormones* or animal byproducts in the feed.”
Theo Weening, the national meat buyer for Whole Foods Market, says he “can assure our customers that our standard is: No antibiotics, EVER! We work very hard to make sure that the people who produce our meat have raised their animals without the use of antibiotics, growth hormones* or animal byproducts in the feed.”