I’m nervous this is not peer-reviewed, has a small sample size, but thought I’d share anyway.
I’ve never fed any of my pets a raw-food diet.
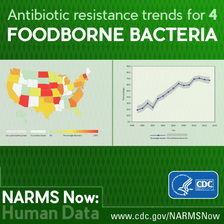
 New research due to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) reveals that raw-type dog foods contain high levels of multidrug-resistant bacteria, including those resistant to last-line antibiotics. The potential transfer of such bacteria between dogs and humans is an international public health risk, conclude the authors who include Dr. Ana Raquel Freitas and colleagues from the Faculty of Pharmacy, UCIBIO/REQUIMTE, University of Porto, Portugal.
New research due to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) reveals that raw-type dog foods contain high levels of multidrug-resistant bacteria, including those resistant to last-line antibiotics. The potential transfer of such bacteria between dogs and humans is an international public health risk, conclude the authors who include Dr. Ana Raquel Freitas and colleagues from the Faculty of Pharmacy, UCIBIO/REQUIMTE, University of Porto, Portugal.
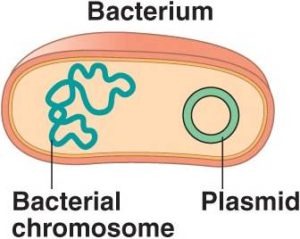
Enterococci are opportunistic pathogens—so they are part of our normal internal microbiota but can cause infections (for example in patients who are immunosuppressed or hospitalised).
Raw-food-based diets for dogs have grown popularity recently as a healthier choice. Increasing controversy regarding their safety is emerging, with some scientific evidence showing their role as vehicles for transmission of antibiotic-resistant bacteria. In addition, dogs have been described as reservoirs of clinically-relevant ampicillin-resistant (AmpR) Enterococcus faecium, but the source remains unknown.
 In this study, the authors analysed enterococci obtained from processed (both dry and wet types) and non-processed (raw-frozen) foods of the main brands commercialised in Portugal. The study included 46 samples (22 wet, 15 dry, 9 raw-frozen) from 24 international brands, sourced from 8 supermarkets and one veterinary clinic. Samples were obtained during September to November, 2019.
In this study, the authors analysed enterococci obtained from processed (both dry and wet types) and non-processed (raw-frozen) foods of the main brands commercialised in Portugal. The study included 46 samples (22 wet, 15 dry, 9 raw-frozen) from 24 international brands, sourced from 8 supermarkets and one veterinary clinic. Samples were obtained during September to November, 2019.
Raw-frozen samples were mainly constituted of salmon, chicken, turkey, calf, deer or duck, being a mixture of different meat types, fruits and vegetables.
Samples were cultured and then tested with a range of antibiotics. Enterococci (n=163) were identified in 19/46 (41%) of the samples: 8 of 15 (53%) in the dry foods; 2 of 22 (9%) of the wet samples, and 9 of 9 (100%) in the raw-frozen samples, and identified as the Enterococcus species E. faecium (91 isolates), E. faecalis (59 isolates) or other species (13 isolates).
Across the 9 raw-frozen meat samples, there were 30 E. faecium and 30 E. faecalis recovered. All nine carried multidrug-resistant (MDR) enterococci (20 E. faecium and 22 E. faecalis), including those resistant to a wide range of antibiotics, while only one MDR- E. faecium (resistant to erythromycin/tetracycline/gentamicin) was detected in one of the wet food samples and none in the dry food samples.
 Resistance was found to the antibiotics ampicillin, ciprofloxacin, erythromycin, tetracycline, streptomycin and chloramphenicol in all 9 raw-type samples; seven of nine contained enterococci resistant to the last line antibiotic linezolid (78%), and six of nine contained enterococci resistant to gentamicin or quinupristin-dalfopristin. Resistance to clinically-relevant antibiotics such as linezolid, ampicillin or ciprofloxacin was only detected in raw-frozen samples.
Resistance was found to the antibiotics ampicillin, ciprofloxacin, erythromycin, tetracycline, streptomycin and chloramphenicol in all 9 raw-type samples; seven of nine contained enterococci resistant to the last line antibiotic linezolid (78%), and six of nine contained enterococci resistant to gentamicin or quinupristin-dalfopristin. Resistance to clinically-relevant antibiotics such as linezolid, ampicillin or ciprofloxacin was only detected in raw-frozen samples.
The authors conclude: “Our study demonstrates that raw-frozen-foods for dogs carry MDR enterococci including to last-line antibiotics (linezolid) for the treatment of human infections. The close contact of pets with humans and the commercialisation of the studied brands in different EU countries pose an international public health risk if transmission of such strains occurs between dogs and humans. There is strong past and recent evidence that dogs and humans share common multidrug-resistant strains of E. faecium, and thus the potential for these strains to be transmitted to humans from dogs.”
Dr. Freitas adds: “These raw-frozen foods are supposed to be consumed after being thawed and could at least be cooked, to kill these drug-resistant and other bacteria. Although these foods seem to be regulated regarding their microbiological safety by EU authorities, risk assessment of biological hazards should also include antibiotic-resistant bacteria and/or genes besides only establishing the presence of bacterial pathogens, such as Salmonella.”