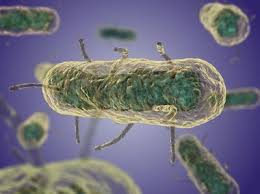
Russ Bynum of Federal News Radio reports that in November 2006, the U.S. Centers for Disease Control and state health officials began investigating an outbreak of salmonella infections ultimately blamed for sickening at least 625 people in 47 states and killing nine.
 Investigators traced the salmonella to jars of Peter Pan and Great Value brand peanut butter produced in Sylvester, Georgia.
Investigators traced the salmonella to jars of Peter Pan and Great Value brand peanut butter produced in Sylvester, Georgia.
ConAgra officials blamed moisture from a leaky roof and a malfunctioning sprinkler system at the Georgia plant for helping salmonella bacteria grow on raw peanuts.
ConAgra launched a huge recall in February 2007, destroying and urging consumers to throw out all of its peanut butter produced since 2004.
Peter Pan peanut butter vanished from store shelves for months. Meanwhile, ConAgra spent $275 million on upgrades at the Georgia plant and adopted new testing procedures to screen peanut butter for contaminants.
Six months later, in August 2007, ConAgra announced it was ready for Peter Pan to return to supermarkets.
Today, ConAgra faces a court hearing to finalize an $11.2 million settlement — including the largest criminal fine ever in a U.S. food safety case — to resolve federal charges in a salmonella outbreak that sickened hundreds who ate tainted Peter Pan peanut butter.
A federal criminal investigation followed the outbreak. More than eight years after the Peter Pan recall, in May 2015, the Justice Department announced charges and a pre-arranged plea deal with ConAgra.
The agreement called for ConAgra Grocery Products Company, a ConAgra subsidiary, to plead guilty to a single misdemeanor charge of shipping adulterated food. No charges were brought against executives of ConAgra, which was based in Omaha, Nebraska, at the time but has since moved its headquarters to Chicago.
ConAgra issued a statement saying the company didn’t know its peanut butter was contaminated with salmonella before it was shipped. However, the plea agreement documents note that ConAgra knew peanut butter made in Georgia had twice tested positive for salmonella in 2004. Prosecutors said the company destroyed the tainted peanut butter and identified likely sources of contamination, but ConAgra had not finished fixing those problems by the time of the 2007 outbreak.