Public health officials in four Canadian provinces are investigating a salmonella outbreak linked to frozen raw breaded chicken products.
 Thirteen cases have been reported, including seven in Ontario, two in Quebec, two in New Brunswick and two in Nova Scotia.
Thirteen cases have been reported, including seven in Ontario, two in Quebec, two in New Brunswick and two in Nova Scotia.
All incidents occurred between June and August and four people required hospitalization, but no deaths have been reported.
Nice timely reporting.
A news release issued by the Public Health Agency of Canada outbreak does not link the outbreak to a particular brand.
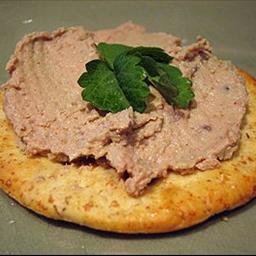
The agency said the outbreak is a reminder that frozen raw breaded poultry products such as nuggets, strips and burgers should be handled the same as other raw poultry products.
“Follow cooking instructions carefully and verify the internal cooking temperature after cooking, as recommended, before consuming these products,” the agency said.
An internal temperature of at least 74 C (165°F) should be reached before eating such products.
The agency said frozen raw breaded chicken products may look pre-cooked, but they contain raw poultry and must be cooked correctly.
Been there, done that.
As we found back in 2007, when preparing frozen foods, adolescents are less likely than adults to wash their hands and are more susceptible to cross-contaminating raw foods while cooking.
“While half of the adults we observed washed their hands after touching raw chicken, none of the adolescents did,” said Casey Jacob, a food safety research assistant at Kansaas State. “The non-existent hand washing rate, combined with certain age-specific behaviors like hair flipping and scratching in a variety of areas, could lead directly to instances of cross-contamination compared to the adults.”
Food safety isn’t simple, and instructions for safe handling of frozen chicken entrees or strips are rarely followed by consumers despite their best intentions, said Doug Powell, K-State associate professor of food safety who led the study.
As the number and type of convenience meal solutions increases — check out the frozen food section of a local supermarket — the researchers found a need to understand how both adults and adolescents are preparing these products and what can be done to enhance the safety of frozen foods.
In 2007, K-State researchers developed a novel video capture system to observe the food preparation practices of 41 consumers – 21 primary meal preparers and 20 adolescents – in a mock domestic kitchen using frozen, uncooked, commercially available breaded chicken products. The researchers wanted to determine actual food handling behavior of these two groups in relation to safe food handling practices and instructions provided on product labels. Self-report surveys were used to determine whether differences exist between consumers’ reported food handling practices and observed behavior.
 The research appeared in the November 2009 issue of the British Food Journal. In addition to Jacob and Powell, the authors were: Sarah DeDonder, K-State doctoral student in pathobiology; Brae Surgeoner, Powell’s former graduate student; Benjamin Chapman, an assistant professor at North Carolina State University and Powell’s former graduate student; and Randall Phebus, K-State professor of animal science and industry.
The research appeared in the November 2009 issue of the British Food Journal. In addition to Jacob and Powell, the authors were: Sarah DeDonder, K-State doctoral student in pathobiology; Brae Surgeoner, Powell’s former graduate student; Benjamin Chapman, an assistant professor at North Carolina State University and Powell’s former graduate student; and Randall Phebus, K-State professor of animal science and industry.
Beyond the discrepancy between adult and adolescent food safety practices, the researchers also found that even when provided with instructions, food preparers don’t follow them. They may not have even seen them or they assume they know what to do.
“Our results suggest that while labels might contain correct risk-reduction steps, food manufacturers have to make that information as compelling as possible or it will be ignored,” Chapman said.
They also found that observational research using discreet video recording is far more accurate than self-reported surveys. For example, while almost all of the primary meal preparers reported washing hands after every instance in which they touched raw poultry, only half were observed washing hands correctly after handling chicken products in the study.
Powell said that future work will examine the effectiveness of different food safety labels, messages and delivery mechanisms on consumer behavior in their home kitchens.
Self-reported and observed behavior of primary meal preparers and adolescents during preparation of frozen, uncooked, breaded chicken products
01.nov.09
British Food Journal, Vol 111, Issue 9, p 915-929
Sarah DeDonder, Casey J. Jacob, Brae V. Surgeoner, Benjamin Chapman, Randall Phebus, Douglas A. Powell
http://www.emeraldinsight.com/Insight/viewContentItem.do;jsessionid=6146E6AFABCC349C376B7E55A3866D4A?contentType=Article&contentId=1811820
Abstract:
Purpose – The purpose of the present study was to observe the preparation practices of both adult and young consumers using frozen, uncooked, breaded chicken products, which were previously involved in outbreaks linked to consumer mishandling. The study also sought to observe behaviors of adolescents as home food preparers. Finally, the study aimed to compare food handler behaviors with those prescribed on product labels.
Design/methodology/approach – The study sought, through video observation and self-report surveys, to determine if differences exist between consumers’ intent and actual behavior.
Findings – A survey study of consumer reactions to safe food-handling labels on raw meat and poultry products suggested that instructions for safe handling found on labels had only limited influence on consumer practices. The labels studied by these researchers were found on the packaging of chicken products examined in the current study alongside step-by-step cooking instructions. Observational techniques, as mentioned above, provide a different perception of consumer behaviors.
Originality/value – This paper finds areas that have not been studied in previous observational research and is an excellent addition to existing literature.
 On Sept. 28, the department issued a public health notice advising people not to consume the dairy’s products.
On Sept. 28, the department issued a public health notice advising people not to consume the dairy’s products.