I was wrong.
When I said Australia is about 20 years behind North America in micro food safety terms, I really meant 40, because that’s when the Brisbane-raised Bee Gees were on the charts with Saturday Night Fever.
 When it comes to public disclosure and on-farm food safety of fresh produce, Australia is only 20 years behind North America.
When it comes to public disclosure and on-farm food safety of fresh produce, Australia is only 20 years behind North America.
It was 1998 when I and many in my lab started working on this problem.
What I soon realized is that government doesn’t give a shit. As sales of an implicated commodity collapse because of a real or imagined outbreak of foodborne illness, the bureaucrats keep their jobs.
Farms go bankrupt.
With 4 dead and 17 sick from Listeria in rockmelon (cantaloupe), this notion has occurred to at least one Western Australian melon grower who is rightly pissed about the lack of information from government, growers, and anyone else.
 Dane Capogreco, one of the directors of Capogreco Farms in Western Australia says the incident is an isolated case of “negligence” and the whole of the country’s melon industry should not be judged by the actions of one grower.
Dane Capogreco, one of the directors of Capogreco Farms in Western Australia says the incident is an isolated case of “negligence” and the whole of the country’s melon industry should not be judged by the actions of one grower.
“The vast majority of growers are doing the right thing. One grower has done the wrong thing and the rest of us are paying the price.”
“It’s very concerning that the grower responsible (from the New South Wales Riverina region) hasn’t come forward to take action,” Mr Capogreco said. “He knew that he had it, and has destroyed the industry. I don’t believe it’s spreadable but it probably happened through the way he handled or washed the fruit post-harvest”
“It (previously) was very good – Australia had a good name. We have a clean, green product. We can’t compete on price alone, but we sell on trust because of our name. Now one guy has set us back a long way.”
He added that his company’s test results are on their website.
That’s a good claim, and something I’ve endorsed for 20 years, but a visit to the website found no such data available, just an eternal circle click.
Something about throwing stones from glass houses.
And again, the Colorado farm in the 2011 Listeria in cantaloupe that killed 33 and sickened at least 140 people in 26 states received a score of 96% in a third-party audit completed by Primus Labs only six days prior to the first reported illness.
Growers, take microbial food safety into your own hands (literally) and be able to prove your product is safe.
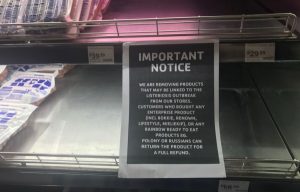
Retailers, market microbial food safety at retail.
Then consumers can choose.
(Me and the ex saw the Dead perform these two songs, pretty much exactly as shown, north of Toronto in 1987 with a six-week old kid, who will turn 31 later this year. I still get goosebumps from their rendition of Buddy Holly’s Not Fade Away)








