In October, 1996, a 16-month-old Denver girl drank Smoothie juice manufactured by Odwalla Inc. of Half Moon Bay, California. She died several weeks later; 64 others became ill in several western U.S. states and British Columbia after drinking the same juices, which contained unpasteurized apple cider — and E. coli O157:H7. Investigators believed that some of the apples used to make the cider might have been insufficiently washed after falling to the ground and coming into contact with deer feces (Powell and Leiss, 1997) not that washing would do much.
 Almost 10 years later, on Sept. 14, 2006, the U.S. Food and Drug Administration announced that an outbreak of E. coli O157: H7 had killed a 77-year-old woman and sickened 49 others (United States Food and Drug Administration, 2006). The outbreak ultimately killed four and sickened at least 200 across the U.S. This was documented-outbreak 29 linked to leafy greens, but also apparently the tipping point for growers to finally get religion about commodity-wide food safety, following the way of their farmer friends in California, 10 years later.
Almost 10 years later, on Sept. 14, 2006, the U.S. Food and Drug Administration announced that an outbreak of E. coli O157: H7 had killed a 77-year-old woman and sickened 49 others (United States Food and Drug Administration, 2006). The outbreak ultimately killed four and sickened at least 200 across the U.S. This was documented-outbreak 29 linked to leafy greens, but also apparently the tipping point for growers to finally get religion about commodity-wide food safety, following the way of their farmer friends in California, 10 years later.
In the decade between these two watershed outbreaks, almost 500 outbreaks of foodborne illness involving fresh produce were documented, publicized and led to some changes within the industry, yet what author Malcolm Gladwell would call a tipping point — “a point at which a slow gradual change becomes irreversible and then proceeds with gathering pace” — in public awareness about produce-associated risks) did not happen until the spinach E. coli O157:H7 outbreak in the fall of 2006. At what point did sufficient evidence exist to compel the fresh produce industry to embrace the kind of change the sector has heralded since 2007? And at what point will future evidence be deemed sufficient to initiate change within an industry?
The 1993 outbreak of E. coli O157:H7 associated with undercooked hamburgers at the Jack-in-the-Box fast food chain propelled microbial food safety to the forefront of public awareness, at least in the U.S. (Powell and Leiss, 1997). In 1996, following extensive public and political discussions about microbial food safety in meat, the focus shifted to fresh fruits and vegetables, following an outbreak of Cyclospora cayetanesis ultimately linked to Guatemalan raspberries that sickened 1,465 in 21 U.S. states and two Canadian provinces (U.S. Centers for Disease Control and Prevention, 1997). That same year, Beuchat (1996) published a review on pathogenic microorganisms in fresh fruits and vegetables and identified numerous pathways of contamination.
 By 1997, researchers at CDC were stating that pathogens could contaminate at any point along the fresh produce food chain — at the farm, processing plant, transportation vehicle, retail store or foodservice operation and the home — and that by understanding where potential problems existed, it was possible to develop strategies to reduce risks of contamination (Tauxe et al., 1997). Researchers also reported that the use of pathogen-free water for washing would minimize risk of contamination (Suslow, 1997; Beuchat, 1998).
By 1997, researchers at CDC were stating that pathogens could contaminate at any point along the fresh produce food chain — at the farm, processing plant, transportation vehicle, retail store or foodservice operation and the home — and that by understanding where potential problems existed, it was possible to develop strategies to reduce risks of contamination (Tauxe et al., 1997). Researchers also reported that the use of pathogen-free water for washing would minimize risk of contamination (Suslow, 1997; Beuchat, 1998).
Beuchat and Ryu (1997) reported in a review that sources of pathogenic microorganisms for produce included:
Preharvest
- Feces
- Soil
- Irrigation water
- Water used to apply fungicides, insecticides
- Green or inadequately composted manure
- Air (dust)
- Wild and domestic animals (including fowl and reptiles)
- Insects
- Human handling
Postharvest
- Feces
- Human handling (workers, consumers)
- Harvesting equipment
- Transport containers (field to packing shed)
- Wild and domestic animals (including fowl and reptiles)
- Insects
- Air (dust)
- Wash and rinse water
- Sorting, packing, cutting, and further processing equipment
- Ice
- Transport vehicles
- Improper storage (temperature, physical environment)
- Improper packaging (including new packaging technologies)
- Cross-contamination (other foods in storage, preparation, and display areas)
- Improper display temperature.
kFresh fruits and vegetables were identified as the source of several outbreaks of foodborne illness in the early 1990s, especially leafy greens (Table 1).
| Date |
Product |
Pathogen |
Cases |
Setting/dish |
State |
| Apr-92 |
Lettuce |
S. enteriditis |
12 |
Salad |
VT |
| Jan-93 |
Lettuce |
S. Heidelberg |
18 |
Restaurant |
MN |
| Jul-93 |
Lettuce |
Norovirus |
285 |
Restaurant |
IL |
| Aug-93 |
Salad |
E. coli O157:H7 |
53 |
Salad Bar |
WA |
| Jul-93 |
Salad |
E. coli O157:H7 |
10 |
Unknown |
WA |
| Sep-94 |
Salad |
E. coli O157:H7 |
26 |
School |
TX |
| Jul-95 |
Lettuce |
E. coli O153:H48 |
74 |
Lettuce |
MT |
| Sep-95 |
Lettuce |
E. coli O153:H47 |
30 |
Scout Camp |
ME |
| Sep-95 |
Salad |
E. coli O157:H7 |
20 |
Ceasar Salad |
ID |
| Oct-95 |
Lettuce |
E. coli O153:H46 |
11 |
Salad |
OH |
| May-96 |
Lettuce |
E. coli O157:H10 |
61 |
Mesclun Mix |
ML |
| Jun-96 |
Lettuce |
E. coli O153:H49 |
7 |
Mesclun Mix |
NY |
Outbreaks of foodborne illness related to leafy greens, 1992-1996.
Dave Gombas told an International Association for Food Protection symposium on leafy green safety on Oct. 6, 2006 in Washington, D.C. that if growers did everything they were supposed to do — in the form of good agricultural practices — and it was verified, there may be fewer outbreaks. He then said government needs to spend a lot more on research.
Wow. The same person who has vacillated between the Produce Marketing Association and the U.S. Food and Drug Administration for the past couple of decades (all you critics who complain about folks jumping back-and-forth-and-back as part of a genetically-engineered conspiracy may want to look at the all-natural, all-good-for-ya produce sector) pronounced on grower verification in which nothing has been done.
Since we were on the same panel in Washington, in 2006, I asked Gombas, why is the industry calling for more investment in research about the alleged unknowns of microbial contamination of produce when the real issue seems to be on-farm delivery and verification? Hiding behind the unknown is easy, working on verifying what is being done is much harder.
More calls for research.
Nothing on human behavior in a fresh produce environment.
It’s just another case of saying the right things in public, but failing to acknowledge what happens on individual farms. Verification is tough. Auditing may not work, because many of these outbreaks happened on third -party audited operations. Putting growers in a classroom doesn’t work, and there’s no evidence that begging for government oversight yields a product that results in fewer sick people.
In 1999, several more outbreaks of Shiga-toxin producing E. coli (STEC) were linked to leafy greens (Table 2), and the U.S. group, the United Fresh Fruit and Vegetable Association, developed and published HACCP-based food safety guidelines for industry (United Fresh Fruit and Vegetable Association, 1999).
| Date |
Product |
Pathogen |
Cases |
Setting/dish |
State |
| Feb-99 |
Lettuce |
E. coli O157:H9 |
65 |
Restaurant |
NE |
| Jun-99 |
Salad |
E. coli O111:H8 |
58 |
Texas Camp |
TX |
| Sep-99 |
Lettuce |
E. coli O157:H11 |
6 |
Iceberg |
WA |
| Oct-99 |
Lettuce |
E. coli O157:H7 |
40 |
Nursing Home |
PA |
| Oct-99 |
Lettuce |
E. coli O157:H7 |
47 |
Restaurant |
OH |
| Oct-99 |
Salad |
E. coli O157:H7 |
5 |
Restaurant |
OR |
Table 2. 1999 U.S. outbreaks of STEC linked to leafy greens
By 2000, Rafferty and colleagues demonstrated that E. coli could spread on-farm in plant production cuttings from one contaminated source, magnifying an outbreak to a whole farm (Rafferty et al., 2000). A 2001 outbreak of Shigella flexneri (886 ill) in tomatoes further focused public and scientific attention onto fresh produce.
Solomon and colleagues (2002a) discovered that the transmission of E. coli O157:H7 to lettuce was possible through both spray and drip irrigation. They also found that the pathogen persisted on the plants for 20 days following application and submerging the lettuce in a solution of 200ppm chlorine did not eliminate all viable E.coli O157:H7 cells, suggesting that irrigation water of unknown microbial quality should be avoided in lettuce production (Solomon et al., 2002a). In a follow-up experiment, Solomon and colleagues (2002b) explored the transmission of E. coli O157:H7 from manure-contaminated soil and irrigation water to lettuce plants. The researchers recovered viable cells from the inner tissues of the lettuce plants and found that the cells migrated to internal locations in plant tissue and were thus protected from the action of sanitizing agents. These experiments demonstrated that E. coli O157:H7 could enter the lettuce plant through the root system and migrate throughout the edible portion of the plant (Solomon et al., 2002b). Such results were widely reported in general media.
During this time, several outbreaks of E. coli were again linked to lettuce and salad (Table 3).
| Date |
Product |
Pathogen |
Cases |
Setting/dish |
State |
| Oct-00 |
Salad |
E. coli O157:H7 |
6 |
Deli |
IN |
| Nov-01 |
Lettuce |
E. coli O157:H7 |
20 |
Restaurant |
TX |
| Jul-02 |
Lettuce |
E. coli O157:H8 |
55 |
Bagged, Tossed |
WA |
| Nov-02 |
Lettuce |
E. coli O157:H7 |
13 |
Restaurant |
IL |
| Dec-02 |
Lettuce |
E. coli O157:H7 |
3 |
Restaurant |
MN |
Table 3: Leafy green outbreaks of STEC, 2000 — 2002.
In 2003, according to Mexican growers, the market impact of an outbreak of hepatitis A traced to exported green onions lasted up to 4 months while prices fell 72 per cent (Calvin et al., 2004). Roma tomatoes were identified as the source of a salmonellosis outbreak that resulted in over 560 cases in both Canada and the US (CDC 2005).
During 2003-2005, several additional outbreaks of E. coli O157:H7 were linked to fresh leafy greens, including one multi-state outbreak involving Dole bagged lettuce (Table 4).
| Date |
Product |
Pathogen |
Cases |
Setting/dish |
State |
| Sep-03 |
Lettuce |
E. coli O157:H7 |
51 |
Restaurant |
CA |
| Nov-03 |
Spinach |
E. coli O157:H7 |
16 |
Nursing Home |
CA |
| Nov-04 |
Lettuce |
E. coli O157:H7 |
6 |
Restaurant |
NJ |
| Sep-05 |
Lettuce |
E. coli O157:H7 |
11 |
Dole, bagged |
Multiple |
Table 4: Leafy green STEC outbreaks, 2003 — 2005.
During 2005–2006, four large multistate outbreaks of Salmonella infections associated with eating raw tomatoes at restaurants occurred in the U.S., resulting in 459 culture-confirmed cases of salmonellosis in 21 states. Investigations determined that the tomatoes had been supplied to restaurants either whole or precut from tomato fields in Florida, Ohio, and Virginia (CDC, 2006).
Allwood and colleagues (2004) examined 40 items of fresh produce taken from a retail setting in the U.S. that had been preprocessed (including cut, shredded, chopped or peeled) at or before the point of purchase. They found fecal contamination indicators (E. coli, F-specific coliphages, and noroviruses) were present in 48 per cent of samples.
Researchers in Minnesota conducted a small-scale comparative study of organic versus conventionally grown produce. They found that while all samples were virtually free of pathogens, E. coli was 19 times more prevalent on produce acquired from the organic farms (Mukherjee et al., 2004). They estimated that this was due to the common use of manure aged for less than a year. Use of cattle manure was found to be of higher risk as E. coli was found 2.4 times more often on farms using it than other animal manures (Mukherjee et al., 2004).
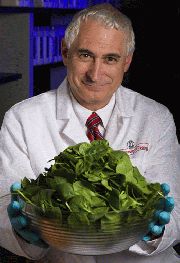
On Sept. 14, 2006, the U.S. Food and Drug Administration (2006) issued a public statement warning against the consumption of bagged fresh spinach.
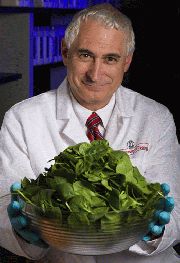
“Given the severity of this illness and the seriousness of the outbreak,” stated Dr. Robert Brackett, Director of FDA’s Center for Food Safety and Applied Nutrition (CFSAN), “FDA believes that a warning to consumers is needed (United States Food and Drug Administration, 2006).”
That is no different from the sometimes conflicting messages coming from FDA today about the E. coli O157:H7 outbreak on lettuce that originated in Yuma, Arizona: these public health folks are figuring it out on the go.
Sean Rossman of USA Today reports today that in the current E. coli O157:H7 outbreak linked to Yuma lettuce, 70% of those who’ve gotten sick are female.
Similarly, when leafy greens were the culprit of an E. coli outbreak last year, 67% of those infected were women or girls. In 2016, females were 73% of those ill from an outbreak in alfalfa sprouts, notes the U.S. Centers for Disease Control and Prevention.
Here are some suggestions:
- The first line of defense is the farm, not the consumer.
- All ruminants — cows, sheep, goats, deer — can carry dangerous E. coli like the O157:H7 strain that sickened people in the spinach outbreak, as well as the Taco Bell and Taco Johns outbreaks ultimately traced to lettuce.
- Any commodity is only as good as its worst grower.
We’ve had a few peer-reviewed thoughts on these topics:
Powell, D.A. and Chapman, B. 2007. Fresh threat: what’s lurking in your salad bowl?. Journal of the Science of Food and Agriculture. 87: 1799-1801.
Implementing On-Farm Food Safety Programs in Fruit and Vegetable Cultivation, Improving the Safety of Fresh Fruit and Vegetables
Luedtke, A., Chapman, B. and Powell, D.A. 2003. Implementation and analysis of an on-farm food safety program for the production of greenhouse vegetables. Journal of Food Protection. 66:485-489.
Powell, D.A., Bobadilla-Ruiz, M., Whitfield, A. Griffiths, M.G.. and Luedtke, A. 2002. Development, implementation and analysis of an on-farm food safety program for the production of greenhouse vegetables in Ontario, Canada. Journal of Food Protection. 65: 918- 923.
A listing of 78 outbreaks linked to leafy greens since 1995 is posted here.
 Ancient latrines found in Bahrain, Jordan, Denmark, the Netherlands, and Lithuania are the focus of the new paper, authored by a team of Danish and Dutch scientists. The samples of ancient waste range significantly in age, with the oldest, found in Bahrain, dating to 500 B.C. to the most recent, found in the Netherlands, dating to 1700 A.D. Microscopy techniques allowed them to pinpoint parasite eggs within the old poop, and DNA analysis of those parasites revealed not only what these humans ate but also the animals they interacted with and the parasites that plagued their stomachs.
Ancient latrines found in Bahrain, Jordan, Denmark, the Netherlands, and Lithuania are the focus of the new paper, authored by a team of Danish and Dutch scientists. The samples of ancient waste range significantly in age, with the oldest, found in Bahrain, dating to 500 B.C. to the most recent, found in the Netherlands, dating to 1700 A.D. Microscopy techniques allowed them to pinpoint parasite eggs within the old poop, and DNA analysis of those parasites revealed not only what these humans ate but also the animals they interacted with and the parasites that plagued their stomachs.