Animal petting zoos and farm fairs provide the opportunity for children and adults to interact with animals, but contact with animals carries a risk of exposure to zoonotic pathogens and antimicrobial‐resistant bacteria.
 The aim of this study was to assess the occurrence of Shiga toxin‐producing Escherichia coli (STEC), Salmonella, extended‐spectrum β‐lactamase (ESBL)‐producing Enterobacteriaceae and methicillin‐resistant Staphylococcus aureus (MRSA) in animal faeces from six animal petting zoos and one farm fair in Switzerland. Furthermore, hygiene facilities on the venues were evaluated.
The aim of this study was to assess the occurrence of Shiga toxin‐producing Escherichia coli (STEC), Salmonella, extended‐spectrum β‐lactamase (ESBL)‐producing Enterobacteriaceae and methicillin‐resistant Staphylococcus aureus (MRSA) in animal faeces from six animal petting zoos and one farm fair in Switzerland. Furthermore, hygiene facilities on the venues were evaluated.
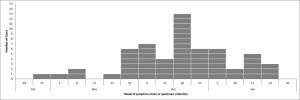
Of 163 faecal samples, 75 contained stx1, stx2 or stx1/stx2 genes, indicating the presence of STEC. Samples included faeces from sika deer (100%), sheep (92%), goats (88%), mouflons (80%), camels (62%), llamas (50%), yaks (50%), pigs (29%) and donkeys (6%), whereas no stx genes were isolated from faeces of calves, guinea pigs, hens, ostriches, ponies, zebras or zebus. Salmonella enterica subsp. enterica serovar Stourbridge (S. Stourbridge) was detected in faecal samples from camels. A total of four ESBL‐producing E. coli strains were isolated from faeces of goats, camels and pigs. PCR and sequencing identified the presence of blaCTX‐M‐15 in three and blaCTX‐M‐65 in one E. coli. Antimicrobial resistance profiling using the disk diffusion method revealed two multidrug‐resistant (MDR) E. coli with resistance to ciprofloxacin, gentamicin and azithromycin, all of which are critically important drugs for human medicine. Multilocus sequence typing identified E. coli ST162, E. coli ST2179, extraintestinal high‐risk E. coli ST410 and E. coli ST4553, which belongs to the emerging extraintestinal clonal complex (CC) 648. No MRSA was detected.
On all animal petting venues, there were inadequacies with regard to access to hygiene information and handwashing hygiene facilities. This study provides data that underscore the importance of hygiene measures to minimize the risk of transmission of zoonotic pathogens and MDR, ESBL‐producing E. coli to visitors of animal petting venues.
Animal petting zoos as sources of shiga toxin-producing Escherichia coli, salmonella and extended-spectrum Beta-lactamase (EXBL)-producing Enterobacteriaceae
Zoonosis and Public Health
Meret Isler, Ramona Wissmann, Marina Morach, Katrin Zurfluh, Roger Stephan, Magdalena Nüesch‐Inderbinen