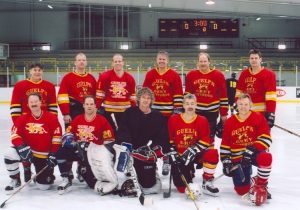
My buddy Scott Weese, whom I haven’t played hockey with for about 15 years (but we won the faculty tournament in 2005, so I figured that was a good time to retire and move to Kansas; I’m the goalie, he’s third from left, back row) writes on his WormsAndGermsBlog that human health risks from raw pet food (either from exposure to pathogens in the food or in the feces of pets eating the food) are known to exist but they’re not well characterized. We know that dogs fed raw meat-based diets clearly have increased risk of shedding various pathogens, particularly Salmonella and multidrug resistant E. coli. We know this results in some degree of disease risk in animals and in humans, but the scope of the problem is poorly understood. A recent report from Public Health England provides some more information about the risks associated with feeding raw pet food.
 The report is about four people who were infected with E coli O157, a particularly nasty strain of E. coli that can cause serious disease in people.
The report is about four people who were infected with E coli O157, a particularly nasty strain of E. coli that can cause serious disease in people.
One person developed hemolytic uremic syndrome (HUS), a particularly severe consequence of infection, and died.
The four cases involved the same strain of E. coli O157. Three individuals had been exposed to dogs fed a raw meat diet. Tripe was the specific ingredient that was implicated.
Samples of raw pet food were collected for testing. All samples from one raw pet food producer were positive for STEC (shiga toxigenic E. coli, the group to which E. coli O157 belongs). A positive test was also obtained from the freezer of one of the affected individuals, and from one sample of raw tripe. It strain isolated from the tripe was a different from the outbreak strain but supported the notion that tripe might have been the cause. It’s not surprising that they couldn’t isolate the outbreak strain from the food, given the lag from the time of exposure of people to the time of sampling of pet food. Contamination is probably sporadic, with different strains contaminating different batches.
Feeding raw meat-based diets is popular, but associated with risks to pets and people (have we said that enough times yet?). My preference is for it not to be done, but I’m realistic enough to know that people are going to do it anyway. So, I focus on two things:
Who should definitely NOT feed raw meat to their pets?
Households where pets or people are at increased risk of severe disease, including those where young, old, pregnant or immunocompromised individuals (human or animal) are present.
If raw meat is to be fed, how can the risk be reduced?
We have a fact sheet on the Worms & Germs Resources – Pets page about how to reduce the risk. In response to this outbreak, Public Health England produced some similar recommendations on handling raw pet food and preventing infections.
Good on ya Scott.
Now, work on driving to the net.












