Twenty years ago, I sent one of my students to a big organic conference in Guelph, and requested that she ask one question: How do you know compost is microbiologically safe?
 The answer was not convincing.
The answer was not convincing.
‘There’s so many good bacteria they out-compete the bad bacteria.’
Fairytale.
Ten years ago, I was visiting a colleague in Melbourne in his high-rise office and he said, see those crappy little houses down there with their crappy little backyard gardens, they provide the produce for Melbourne’s high-end restaurants, and it’s all fertilized with night soil’ (human shit).
A couple of days ago The Packer published a piece about composting food safety.
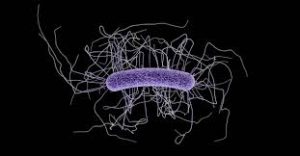
Doug Grant, who chairs the Center for Produce Safety’s Knowledge Transfer Task Force wrote that composting is a seemingly magical process that decomposes organic materials like green waste or animal manures through microbial fermentation, creating nutrient-rich amendments that can be added back to soils.
It’s not magical; it’s microbiological.
However, compost can also pose a risk to the food safety of fresh produce.
Animal manure is widely suspected to be a significant source of human pathogens. Cows can carry E. coli, while poultry and swine can carry Salmonella. If compost is made with manure containing such pathogens, and the composting process is not controlled properly, these pathogens can survive composting. Contaminated compost applied to fields can then cross-contaminate fresh produce that contacts amended soil during growth, irrigation or harvest.
Yes, we have over 20 years of evidence.
Gurmail Mudahar, Ph.D., is vice president of research and development and food safety at Tanimura & Antle and is a member of CPS’s technical committee and California Leafy Greens Marketing Agreement’s (LGMA) advisory board. He reports that his company used to prepare and apply their own animal manure-based composts. That changed when food safety emerged as a major leafy greens industry issue almost two decades ago.
Then Tanimura & Antle and other growers began buying compost only from specialized manufacturers to minimize produce safety hazards.
At its simplest, composting is a manufacuring process. To produce compost safely, the most critical controls are high temperature and time held at that temperature. Over time, the heat generated by microbial respiration in turn reduces the compost’s microbial population, including any human pathogens present.
As a general rule, compost temperatures must reach 131 degrees Fahrenheit or 55 degrees Celsius for 3-15 days, followed by a curing phase of least 21 days and preferably a few months. (Once applied to agricultural fields, pathogens continue to die off when exposed to sunlight’s ultraviolet rays, humidity, temperature, time and other factors.)
Use a thermometer and stick it in.