Some time about 2009, I was walking the dogs on a Sunday morning on the Kansas State University campus with a Canadian graduate student who was getting her MS degree at K-State, and we ran into University president, Jon Wefald.
 We exchanged pleasantries, he was enamored by the dogs, and soon the conversation turned a pet food recall that had sickened dozens of humans with some bad bug.
We exchanged pleasantries, he was enamored by the dogs, and soon the conversation turned a pet food recall that had sickened dozens of humans with some bad bug.
Jon asked me, how are people getting sick from pet food and I explained the sometimes lack of process validation in pet food, the wonderful world of cross-contamination, of and that sometimes people ate pet food directly.
Jon was aghast.
I was, meh.
So that’ why these pet food recalls s are important, because the product can all to easily sicken humans along with their pets.
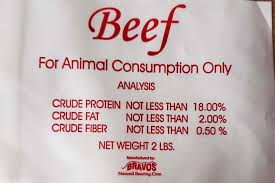
Bravo Packing, Inc. has recalled all Ground Beef and Performance Dog frozen raw pet food because it may be contaminated with bacteria like Salmonella and Listeria monocytogenes.
No illnesses have been reported, but pets who eat the food and people who handle it can become sick with Salmonella and/or Listeria infections.
The recall involves Performance Dog and Ground Beef Raw Pet Food, which are both sold frozen in 2-pound and 5-pound plastic sleeves.
Bravo Packing issued the recall voluntarily after product samples of Performance Dog and a sample of Ground Beef tested positive for Salmonella and Listeria after an FDA inspection.
The FDA warns that pets with Salmonella infections may be lethargic and have diarrhea or bloody diarrhea, fever, vomiting, decreased appetite, abdominal pain, or show no symptoms at all.