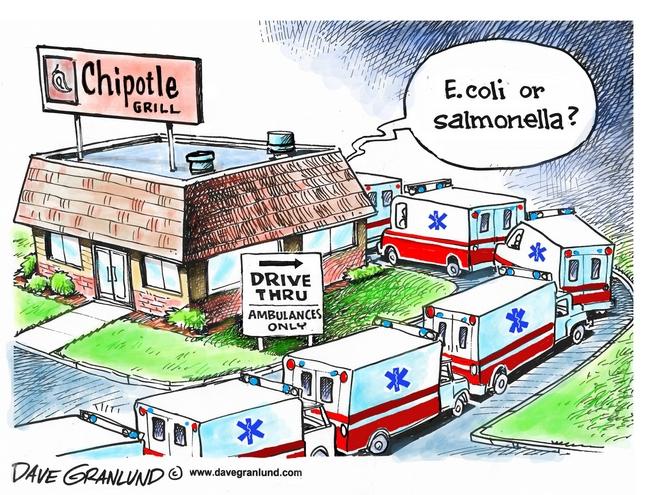
A few years ago an outbreak linked to a Denver homeless shelter made it into the barfblog new and notable category. Forty folks who depended on the emergency food were affected by violent foodborne illness symptoms after eating donated turkey. Fourteen ambulances showed up and took those most affected to area hospitals.
Volunteering as a food handler at a mission, shelter or soup kitchen and having a good heart and intentions doesn’t automatically lead to safe meals. An understanding of risks and having systems how to reduce them may.
Exposing individuals coping with food security and hunger to risky practices isn’t a good humanitarian approach. Last week KOMO News (Seattle) covered the possible closure of a free meal program for food safety reasons:
Every Thursday, Celeste Wilson whips up some of her best recipes. “They say it tastes very good because it’s Chinese food,” she said with a laugh. “It’s not just soup or salad or sandwich. Something different.”
Wilson is one of dozens of volunteers who makes food at home and then serves it at the Issaquah Community Hall.
As many as 80 people attend the free Thursday lunch as well as volunteer provided dinners, which are served seven days a week to countless people.
The diners come for something they wouldn’t have otherwise – a healthy, home cooked meal. But “home cooked” just got the attention of the Public Health of Seattle-King County, which says meals like these must be prepared in a commercial kitchen by someone with food safety certification.
“We don’t like to think of food in that way of having that potential of being the source that could make us sick. But just because we don’t know that someone has gotten sick, doesn’t mean that someone hasn’t. With food it’s very possible,” said Becky Elias, Manager of Food Protection and Water Recreation Programs at Public Health.
Around the same time as the Denver outbreak, colleague, friend and STEC CAP collaborator Christine Bruhn created a set of food safety materials for folks volunteering with food in their communities. Ashley Chaifetz, a former graduate student in the department of public policy at UNC-Chapel Hill took Christine’s content foundation and went out to the food pantry community to assess infrastructure and current food safety practices to tailor materials to the audience.
The assessment work was published in the November issue of the Journal of Food Protection:
Evaluating North Carolina Food Pantry Food Safety–Related Operating Procedures
Ashley Chaifetz, University of North Carolina at Chapel Hill; Benjamin Chapman, North Carolina State University
Journal of Food Protection
Vol. 78, No. 11, 2015, Pages 2033–2042
DOI: 10.4315/0362-028X.JFP-15-084
Abstract: Almost one in seven American households were food insecure in 2012, experiencing difficulty in providing enough food for all their members due to a lack of resources. Food pantries assist a food-insecure population through emergency food provision, but there is a paucity of information on the food safety–related operating procedures that pantries use. Food pantries operate in a variable regulatory landscape; in some jurisdictions, they are treated equivalent to restaurants, while in others, they operate outside of inspection regimes. By using a mixed methods approach to catalog the standard operating procedures related to food in 105 food pantries from 12 North Carolina counties, we evaluated their potential impact on food safety. Data collected through interviews with pantry managers were supplemented with observed food safety practices scored against a modified version of the North Carolina Food Establishment Inspection Report. Pantries partnered with organized food bank networks were compared with those that operated independently. In this exploratory research, additional comparisons were examined for pantries in metropolitan areas versus nonmetropolitan areas and pantries with managers who had received food safety training versus managers who had not. The results provide a snapshot of how North Carolina food pantries operate and document risk mitigation strategies for foodborne illness for the vulnerable populations they serve. Data analysis reveals gaps in food safety knowledge and practice, indicating that pantries would benefit from more effective food safety training, especially focusing on formalizing risk management strategies. In addition, new tools, procedures, or policy interventions might improve information actualization by food pantry personnel.




 Right now there are two outbreaks linked to unpasteurized ciders in
Right now there are two outbreaks linked to unpasteurized ciders in