Forming biofilms may be a survival strategy of Shiga toxin-producing Escherichia coli to enable it to persist in the environment and the food industry.
Here, we evaluate and characterize the biofilm-forming ability of 39 isolates of Shiga toxin-producing Escherichia coli isolates recovered from human infection and belonging to seropathotypes A, B, or C.
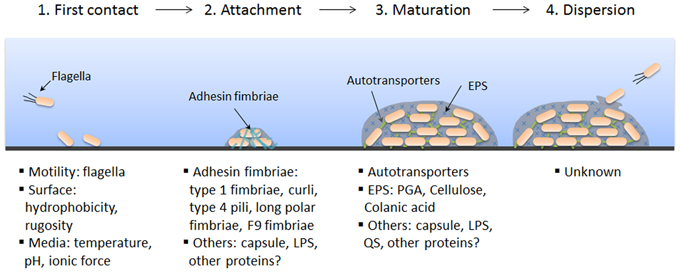
The presence and/or production of biofilm factors such as curli, cellulose, autotransporter, and fimbriae were investigated. The polymeric matrix of these biofilms was analyzed by confocal microscopy and by enzymatic digestion. Cell viability and matrix integrity were examined after sanitizer treatments. Isolates of the seropathotype A (O157:H7 and O157:NM), which have the highest relative incidence of human infection, had a greater ability to form biofilms than isolates of seropathotype B or C. Seropathotype A isolates were unique in their ability to produce cellulose and poly-N-acetylglucosamine.
The integrity of the biofilms was dependent on proteins. Two autotransporter genes, ehaB and espP, and two fimbrial genes, z1538 and lpf2, were identified as potential genetic determinants for biofilm formation. Interestingly, the ability of several isolates from seropathotype A to form biofilms was associated with their ability to agglutinate yeast in a mannose-independent manner. We consider this an unidentified biofilm-associated factor produced by those isolates.
Treatment with sanitizers reduced the viability of Shiga toxin-producing Escherichia coli but did not completely remove the biofilm matrix. Overall, our data indicate that biofilm formation could contribute to the persistence of Shiga toxin-producing Escherichia coli and specifically seropathotype A isolates in the environment.
Biofilm-forming abilities of Shiga toxin-producing Escherichia coli isolates associated with human infections
Applied and Environmental Microbiology Vol. 82. No. 5.