Some shellfish, especially raw oysters, may contain dangerous levels of the pathogen Vibrio parahaemolyticus (Vp), a cousin of the bug that causes cholera.
 When ingested, Vp can cause the food poisoning called vibriosis, which usually entails an unpleasant three days of nausea, diarrhea, fever and chills. In rare cases and among vulnerable populations—the very young, very old or those with weakened immune systems—the bacterium can cause a more serious blood infection. Vp, which can also cause skin infections, leads to about 30 hospitalizations and kills one to two people each year, according to the Centers for Disease Control and Prevention.
When ingested, Vp can cause the food poisoning called vibriosis, which usually entails an unpleasant three days of nausea, diarrhea, fever and chills. In rare cases and among vulnerable populations—the very young, very old or those with weakened immune systems—the bacterium can cause a more serious blood infection. Vp, which can also cause skin infections, leads to about 30 hospitalizations and kills one to two people each year, according to the Centers for Disease Control and Prevention.
In Massachusetts, 58 cases of Vp-related illnesses were reported to the Department of Public Health in 2013, up from 13 cases in 2011. The state banned oyster harvesting in waters off Cape Cod, Martha’s Vineyard and Nantucket as well as off the towns of Plymouth, Kingston, Duxbury and Marshfield that year. The last two years waters in New York, Oregon and Washington State have been closed to oystering.
Vp occurs naturally in most marine ecosystems, but it typically has only been linked to disease in warm coastal areas, such as the Gulf of Mexico. The recent emergence of Vp-associated illness linked to seafood from waters off Alaska, Long Island and Massachusetts has made public health officials and others sit up and take notice, says Meghan Hartwick, who received a master’s degree in conservation medicine from Cummings School in 2012 and now works to predict and control future outbreaks.
 Why has Vp-related illness spread to more northern latitudes? Some scientists speculate it might have to do with climate change and rising ocean temperatures. “When we see these kinds of outbreaks in historically cold-water areas, it’s really unusual,” says Hartwick, who is studying the Vibrio species as a Ph.D. student in biology at the University of New Hampshire.
Why has Vp-related illness spread to more northern latitudes? Some scientists speculate it might have to do with climate change and rising ocean temperatures. “When we see these kinds of outbreaks in historically cold-water areas, it’s really unusual,” says Hartwick, who is studying the Vibrio species as a Ph.D. student in biology at the University of New Hampshire.
Hartwick hopes to develop a predictive mathematical model that can warn public health officials and shellfish growers when Vp outbreaks might occur. She helped implement such an environmental surveillance tool for cholera in Vellore, India, as part of her conservation medicine program at Tufts.
Nationwide, Vibrio parahaemolyticus cases are also on the rise. The Centers for Disease Control reports a 115 percent increase since 1996, when the agency started tracking Vp-associated illnesses. Of the 431 cases the CDC confirmed in 2012, six were fatal. Officials also suspect that Vp is vastly underreported, by as much as tenfold.
Hartwick is studying the Vibrio population in the Great Bay tidal estuary on the New Hampshire coast that empties into the Gulf of Maine. Collaborating with UNH colleagues with expertise in microbial ecology, genetics, molecular evolution and remote sensing, Hartwick is trying to understand the role the bacteria plays within Great Bay’s ecosystem.
The “sole goal [of Vp] in life is not to be a human pathogen,” she says. “Vp is an intrinsic part of the flora and fauna of most marine and estuarine ecosystems.”
In the spring and summer, Hartwick collects water and sediment samples and gathers data about water temperature, salinity, pH levels and anything else that might affect the bacteria’s numbers. Over time, she hopes to map how much and which species of Vibrio bacteria are present in Great Bay during the summer, as well as what factors might promote an outbreak.
In addition to developing a Vibrio early-warning tool, Hartwick and the UNH team, including her advisor, bacteriologist Stephen Jones, are working with shellfish growers to figure out how to prevent future outbreaks. After all, no one wants to sell food that makes people sick, she says.
“We’re not blindly throwing a dart and hoping it solves the problem,” Hartwick says. “We’re asking, ‘What is the problem, and what’s the best way to address it,’ so there are no unnecessary burdens placed on the shellfish industry, and there’s also no unnecessary illness. It’s sustainable science contributing to sustainable policy.”
Now into a second summer of collecting samples in Great Bay, Hartwick says she eventually would like to do work in sustainable development on a global scale. Disrupting ecosystems is one of the surest ways to trigger epidemics, such as cholera, she says, and disease is one of the heaviest economic burdens developing nations have to bear.
“If a developing nation can navigate that, it can jump ahead economically,” she says. “It’s hard for me not to think, ‘How can we conserve the environment and improve human health and the economy and education—everything at once?’ My approach is to minimize disease.”
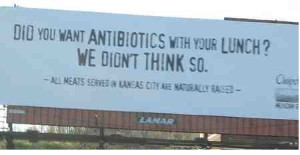
 “Our school meals are healthy, nutritious and safe. And food safety is our top priority,” says Sherrie Johnson, spokeswoman for Prince George’s County Public Schools.
“Our school meals are healthy, nutritious and safe. And food safety is our top priority,” says Sherrie Johnson, spokeswoman for Prince George’s County Public Schools.