Graduate students Nicole Arnold (NC State) and Lily Yang (Virginia Tech) write (below, exactly as shown),
As Dr. Chapman and Dr. Boyer began to delve into the realm of something called “mechanically tenderized beef,” Lily and Nicole glanced apprehensively at each other from across the table. Feeling dwarfed by the immenseness of the Indianapolis Convention Center amidst the hubbub of the the 2014 International Association for Food Protection (IAFP) Annual Meeting, neither of them could have imagined the adventure they were soon to embark upon. What started as a simple question, “Do you want to work with people?” had quickly blossomed and developed into a mind and story of its own. In a world of sensationalized media and fear-mongering, coupled with consumer beliefs of personal immunity, the study of consumer behavior and knowledge has become an essential step toward developing outreach, education, and intervention methods to positively influence consumer behavior changes. However, leaping into science alone can be a scary venture; having a partner-in-crime at one’s side not only makes the experience more fun and exciting, but much less terrifying.
After months of discussion, the multi-faceted goals of their project, under the USDA NIFA STEC-CAP grant, were finally hashed out. Beginning May 2016, a label would be required for mechanically tenderized beef products due to the potential health risk when not fully cooked. As food scientists, it was important for us to better understand these products and to also recognize how consumers and small-scale retailers perceive them. Nicole (working towards a MS at North Carolina State University, NCSU) would determine the prevalence of mechanical tenderization of beef at independent retail markets in North Carolina and Virginia. Lily (working towards a PhD at Virginia Tech, VT) would assess consumer knowledge and behavior towards mechanically tenderized beef through focus groups, nation-wide surveys, and video observations. From these observations and consumer interactions, intervention methods for affecting behavior would be developed, implemented, then evaluated for effectiveness.
As their project is so incredibly people-oriented, networking and making friends within the food safety world became imperative as many will one day become their colleagues. The importance of partnership and collaboration was emphasized from the moment that Nicole began in the Chapman lab at NCSU and Lily began in the Boyer lab at VT. The combined infectious personalities of Nicole’s charm and Lily’s gregarious nature have allowed them to meet, collaborate, and make friends all across the food science community.
The two first began working together over three years ago, when Nicole was still an undergraduate student at NCSU and Lily was a MS student at VT. At the time, their work together was strictly virtual; they pulled news stories for barfblog, a blog used to discuss evidence-based opinions on current food safety issues by many food safety scientists (check it out here: https://barfblog.com/). Many months later at the IFTSA Central Atlantic Area Meeting 2013 at NCSU, Nicole recognized Lily’s incredible loudness while giving the other schools tours of the NC State Howling Cow Dairy. Amidst squeals of excitement and hugs, Nicole also revealed that she would be joining Chapman’s lab for her Master’s studies.
Now, a few years later, Lily and Nicole are great friends. Each has visited the other’s school to work on their shared project; both of their advisors serve on either girls’ committees. Nicole and Lily are frequently involved in many various joint adventures. The two have gone on many adventures at conferences (i.e.: IAFP, IFT, STEC, etc.), in addition to those outside of academia and scientific-related ventures. Recently, Lily took over as the new chair of the IAFP Student Professional Development Group. Nicole serves as the vice-chair. Lily and Nicole were also both accepted into IFT’s first annual Food Communicator’s Workshop in 2015. Along with a group of like-minded young food communicators, they are members of a working group called Don’t Eat the Pseudoscience (You should check them out here on Youtube at http://bit.ly/1KvSNMY and on Facebook at https://www.facebook.com/DontEatPseudo ). This team of students works towards effectively communicating food, science, and all aspects of Food Science through videos, social media, and other prominent channels.
Together, Nicole and Lily hope to share their own positive experiences working with one another and with other students in order to promote more collaboration and teamwork among students interested in food science and food safety. Acknowledging that your own limitations may be another individual’s expertise is essential. The diversity within food science and food safety is something to celebrate. After all, every great adventure begins with two.
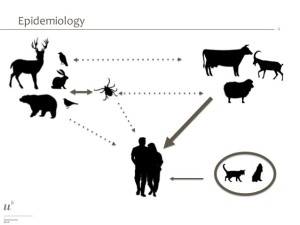
 Acute autochthonous HE cases confirmed by the National Reference Centre (CNR) were interviewed on exposures in the 2 to 10 weeks before illness onset. Clinical, biological and epidemiological characteristics were documented for 139 autochthonous cases.
Acute autochthonous HE cases confirmed by the National Reference Centre (CNR) were interviewed on exposures in the 2 to 10 weeks before illness onset. Clinical, biological and epidemiological characteristics were documented for 139 autochthonous cases.