Consumption of fruit and vegetables is associated with a healthy lifestyle. Various international organizations, such as the World Health Organization, encourage the daily intake of at least 400 g of fruit and vegetables per day (excluding potatoes and other starchy tubers) for the prevention of chronic diseases, such as heart disease, cancer, diabetes, and obesity.
 A large portion of this produce is consumed raw, and the number of foodborne outbreaks associated with these products has increased correspondingly. In this context, unpasteurized fruit juices and raw sprouts are also considered high-risk foods. The 2011 Escherichia coli O104:H4 outbreak from sprouted seeds in Germany gives a clear indication of the emerging relevance of the consumption of these products within food safety issues.
A large portion of this produce is consumed raw, and the number of foodborne outbreaks associated with these products has increased correspondingly. In this context, unpasteurized fruit juices and raw sprouts are also considered high-risk foods. The 2011 Escherichia coli O104:H4 outbreak from sprouted seeds in Germany gives a clear indication of the emerging relevance of the consumption of these products within food safety issues.
Globalization and growing international trade can also increase the risk, especially if produce comes from countries with lower safety standards. Nevertheless, nutrition educators and healthcare professionals believe that the benefits of eating fresh fruits and vegetables outweigh the risk of contracting a foodborne illness by consuming fresh produce.
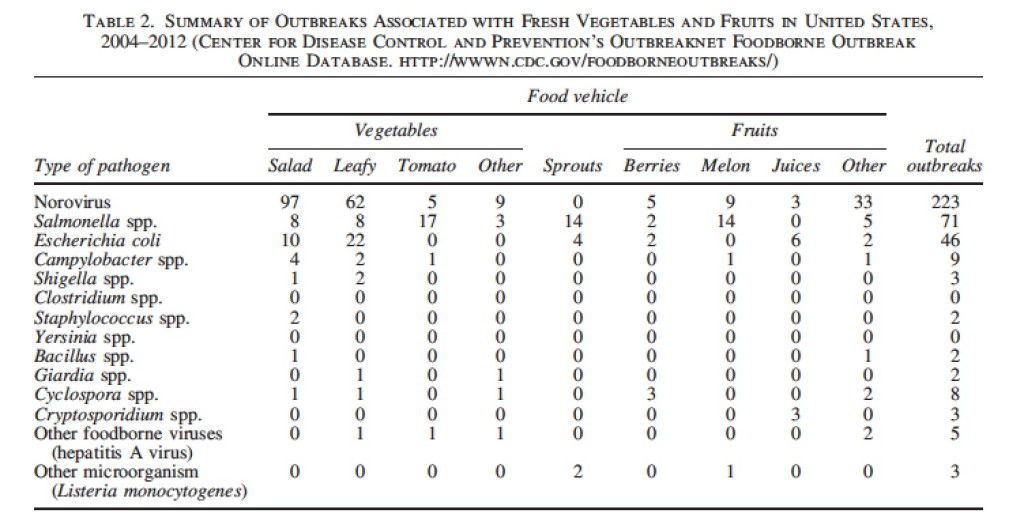
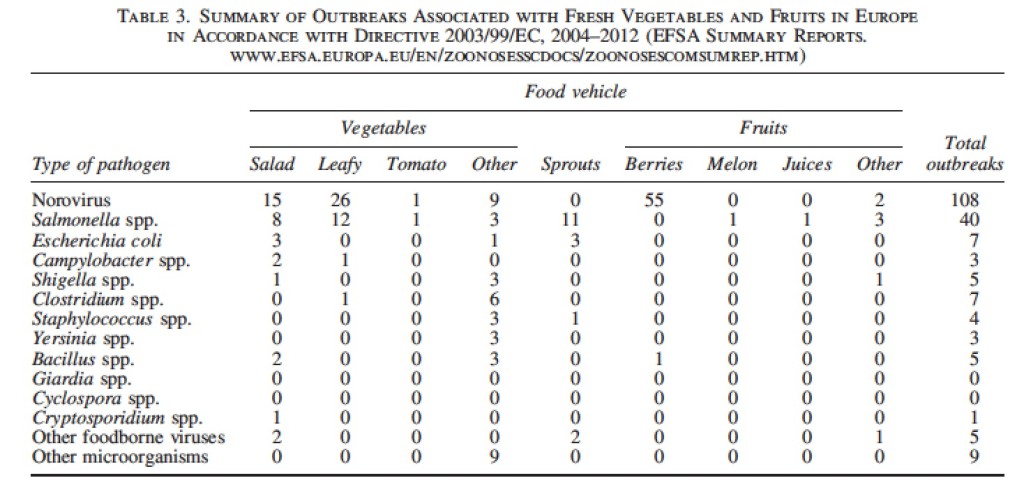
The number of reported outbreaks (defined as the occurrence of two or more cases of similar illness resulting from the ingestion of a common food) reported both in the United States and European Union represents only a fraction of the actual number of outbreaks that occur.
Large outbreaks, outbreaks associated with food service and institutions, and outbreaks that have a longer duration or cause serious disease are more likely to be investigated and reported. Conversely, the data may not reflect what occurs in
sporadic cases. Moreover, there are differences in the sensitivity of the national or state systems in identifying and investigating foodborne outbreaks.
 A wide spectrum of pathogens and food vehicles has been documented in produce-associated outbreaks. The occurrence of food-related infections due to fresh produce calls for better control interventions and the need for improved prevention strategies worldwide, since food can be contaminated at any point in the food chain, and interventions must be applied where appropriate at every step. Hence, the future success of global efforts to prevent produce-related outbreaks depends on the understanding of the key contributing factors and the maintenance of best practices to reduce and eliminate contamination.
A wide spectrum of pathogens and food vehicles has been documented in produce-associated outbreaks. The occurrence of food-related infections due to fresh produce calls for better control interventions and the need for improved prevention strategies worldwide, since food can be contaminated at any point in the food chain, and interventions must be applied where appropriate at every step. Hence, the future success of global efforts to prevent produce-related outbreaks depends on the understanding of the key contributing factors and the maintenance of best practices to reduce and eliminate contamination.
Reported foodborne outbreaks due to fresh produce in the United States and European Union: trends and causes
Foodborne Pathogens and Disease. January 2015, 12(1): 32-38
Callejón Raquel M., Rodríguez-Naranjo M. Isabel, Ubeda Cristina, Hornedo-Ortega Ruth, Garcia-Parrilla M. Carmen, and Troncoso Ana M.
Abstract
The consumption of fruit and vegetables continues to rise in the United States and European Union due to healthy lifestyle recommendations. Meanwhile, the rate of foodborne illness caused by the consumption of these products remains high in both regions, representing a significant public health and financial issue. This study addresses the occurrence of reported foodborne outbreaks associated with fresh fruits and vegetables consumption in the United States and European Union during the period 2004–2012, where data are available. Special attention is paid to those pathogens responsible for these outbreaks, the mechanisms of contamination, and the fresh produce vehicles involved. Norovirus is shown to be responsible for most of the produce-related outbreaks, followed by Salmonella. Norovirus is mainly linked with the consumption of salad in the United States and of berries in the European Union, as demonstrated by the Multiple Correspondence Analysis (MCA). Salmonella was the leading cause of multistate produce outbreaks in the United States and was the pathogen involved in the majority of sprouts-associated outbreaks. As is reflected in the MCA, the pattern of fresh produce outbreaks differed in the United States and European Union by the type of microorganism and the food vehicle involved.