The UK Advisory Committee on the Microbiological Safety of Food (ACMSF) has published its extensive review of viruses in the food chain. The ACMSF set up a group to revisit the issue of foodborne viruses in light of developments in this area. The final report considered the most important viruses associated with foodborne infections – norovirus, hepatitis A, and hepatitis E.
 The report makes a number of recommendations for government departments, including the need for more research in certain areas, and for clear advice for consumers, for example on cooking shellfish and pork products and information on washing leafy green vegetables and soft fruit. The government will respond in due course when the recommendations have been considered in detail.
The report makes a number of recommendations for government departments, including the need for more research in certain areas, and for clear advice for consumers, for example on cooking shellfish and pork products and information on washing leafy green vegetables and soft fruit. The government will respond in due course when the recommendations have been considered in detail.
Professor Sarah O’Brien, Chair of the ACMSF, said: ‘Until recently it has been difficult to assess accurately the impact of foodborne viruses on public health. However, significant advances in our ability to detect viruses in food, coupled with up- to-date estimates of the burden of illness, highlighted in the ACMSF’s latest update, show us that viruses are very important, preventable causes of foodborne illness.’
Summary
In 1994, in response to the outcomes of a joint Advisory Committee of Microbiological Safety of Food (ACMSF) and Steering Group on the Microbiological Safety of Food (SGMSF) meeting, a Working Group was set up to investigate the science and epidemiology of Foodborne Viral Infections. The Working Group assessed the risk from viruses that were believed to be the primary cause of foodborne illness. This report provides an update to this information and provides a new focus on the viruses which are currently the major route of foodborne illness.
Since the publication of the 1998 report, with the exception of two minor risk assessments on hepatitis E and avian influenza, no formal review on viruses had been performed by the ACMSF. It was decided that as significant developments had been made not only in the detection of foodborne viruses, but also in the amount of information obtained from the Infectious Intestinal Disease (IID) Study in England (published in 2000), which indicated a significant disease burden from enteric viruses in the community, it was important that an Ad-Hoc Group was convened to revisit these issues and to provide an update to the 1998 risk assessment.
 The FVI Group first met to begin their consideration in November 2010. Over 32 months, the Group met thirteen times to discuss all aspects of viruses in the food chain from farm to fork. As a starting point for the report, the Group reviewed the recommendations from the 1998 report and gave consideration as to whether these had been adequately addressed or were still relevant. At the same time the recommendations from the 2008 World Health Organisation (WHO) Viruses in Food: Scientific Advice to Support Risk Management Activities Matrix and CODEX Criteria, and the European Food Safety Authority (EFSA) Scientific Opinion on an update on the present knowledge on the occurrence and control of foodborne viruses were reviewed.
The FVI Group first met to begin their consideration in November 2010. Over 32 months, the Group met thirteen times to discuss all aspects of viruses in the food chain from farm to fork. As a starting point for the report, the Group reviewed the recommendations from the 1998 report and gave consideration as to whether these had been adequately addressed or were still relevant. At the same time the recommendations from the 2008 World Health Organisation (WHO) Viruses in Food: Scientific Advice to Support Risk Management Activities Matrix and CODEX Criteria, and the European Food Safety Authority (EFSA) Scientific Opinion on an update on the present knowledge on the occurrence and control of foodborne viruses were reviewed.
Using this information along with data on disease burden in the community and outbreak data (from IID and IID2) the Group agreed the scope of the report and what viruses would be its main focus. It was decided that that due to their potential impact and the paucity of data in this area, norovirus, hepatitis E and hepatitis A would be the main focus of the report, although many of the recommendations would also be applicable to other enteric viruses.
During its consideration, the Group reviewed available data on commodities contaminated at source, i.e. bivalve shellfish, pork products and fresh produce and reviewed data on risks associated with infected food handlers. Environmental contamination was reviewed with consideration given to testing methods such as polymerase chain reaction (PCR), person-to-person transmission and food handlers. The Group also considered the engagement with industry and other Government departments (OGDs) regarding environmental conditions of shellfish waters and its impact on norovirus.
A review of data on issues regarding food contact surface contamination, including survivability and persistence was considered along with options for control at all stages of the food chain e.g. thermal processing, storage etc. The thermal stability of hepatitis E was considered with data presented on the increasing occurrence of the disease particularly in older UK males and the recent case control study on the association with processed pork products.
In order to obtain sentinel data the group investigated the important issue of knowledge gathering and surveillance data regarding foodborne viruses. The current limitations of the data were discussed along with what type of data was needed to provide more useful/accurate information on foodborne virus outbreaks. This review included looking at outbreaks from an Environmental Health Officer (EHO) perspective and how they prioritise what they investigate and the data they collect.
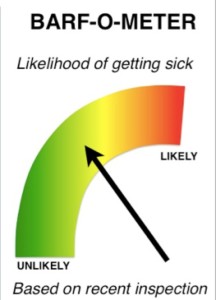
Finally, the group reviewed the consumer perspective on risk. This included looking at how risk is presented and information distributed, as this was likely to impact on any future risk assessment.
Within the report the Group has endeavoured to prioritise the recommendations by separating these into those that will inform risk assessments and those that will impact on risk assessments. Full details are provided in the report; however, key recommendations include:
A better understanding of ‘’foodborne viral disease’ (Chapter 3) is required by investigating the correlation between infective dose and genome titre. Molecular diagnostics, typing and quantification should also be used to better understand the burden of virus contamination in foodstuffs. Work is also recommended to develop the methods used to assess norovirus and hepatitis E infectivity in food samples. This would better inform surveys and could potentially be applied to routine monitoring.
Improved ‘routine surveillance and investigation of foodborne viruses’ (Chapter 5) is required with Government agencies developing a single integrated outbreak reporting scheme. A joined up approach that would also involve the annual consolidation of records would reduce the chance of underreporting outbreaks. Further to this, reliable methods for norovirus whole genome sequencing should be developed to enable virus tracking and attribution.
More research on the ‘contamination of food’ (Chapter 6) through sewage contamination is recommended. In particular work should investigate the effectiveness of sewage treatment processes in reducing norovirus concentrations, including the use of depuration on shellfish species and disinfection treatments. Similarly, research is needed to identify the most effective means of decontaminating ‘fresh produce’ post-harvest (Chapter 7).
With the emerging risk of hepatitis E in pigs, the Group recommends work is undertaken to investigate the heat inactivation of hepatitis E in ‘pork products’ (Chapter 8). Research on the effect of curing and fermentation on hepatitis E in pork products is also recommended.
The full list of conclusions and recommendation are presented at the end of each subject area and are consolidated in Chapter 12 for ease of reference.
The assessments made and conclusions reached by the Group reflect evidence oral and written drawn from the scientific community, Government departments and Agencies, EFSA and the scientific literature. The Group’s full conclusions, identified data gaps and recommendations are brought together at the end of this report. The ACMSF accepts full responsibility for the final content of the report.