Handwashing is simple.
 Science says otherwise.
Science says otherwise.
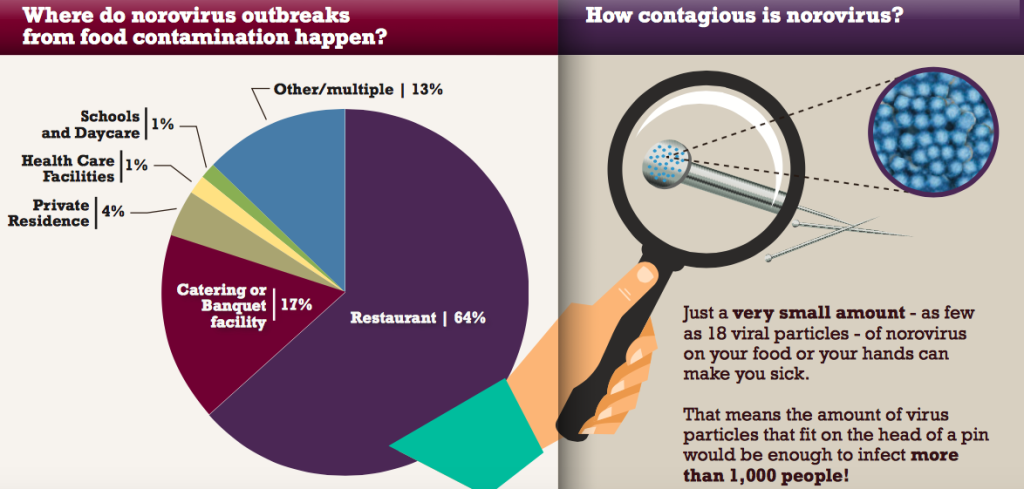
Despite endless statements to just wash hands to be safe — in the kitchen, in food service, at the petting zoo — little research has been done to quantify what actually works when it comes to handwashing.
U.S. government recommendations for 15-20 seconds of handwashing under vigorously flowing water after a potential contamination event may not be practical in a food service environment.
Dr. Donald Schaffner, a professor of food safety at Rutgers University, and colleagues, have attempted to add some science to the discussion.
“Many people seem to have strongly held opinions about handwashing, says Schaffner, “but the research base for those opinions is lacking. Our research begins to dispels some popular beliefs about handwashing.”
The researchers showed that even a minimal handwash (5 seconds, no soap) can remove about 90 per cent of bacteria on hands.
Further, the research showed that towel drying was much more effective than other methods because of the friction involved in physically removing bacteria from hands.
Schaffner says “Everyone has an opinion about handwashing, but our research is beginning to provide real data to help inform sensible policy.”
Contact: Dr. Donald Scaffner
schaffner@aesop.rutgers.edu
732-982-7475
Abstract
Quantifying the effect of hand wash duration, soap use, ground beef debris, and drying methods on the removal of Enterobacter aerogenes on hands
Journal of Food Protection®, Number 4, April 2015, pp. 636-858, pp. 685-690(6)
Jensen, Dane A.;Danyluk, Michelle D.; Harris, Linda J.;Schaffner, Donald W.
http://www.ingentaconnect.com/content/iafp/jfp/2015/00000078/00000004/art00007
Hand washing is recognized as a crucial step in preventing foodborne disease transmission by mitigating cross-contamination among hands, surfaces, and foods.
This research was undertaken to establish the importance of several keys factors (soap, soil, time, and drying method) in reducing microorganisms during hand washing. A nonpathogenic nalidixic acid–resistant Enterobacter aerogenes surrogate for Salmonella was used to assess the efficacy of using soap or no soap for 5 or 20 s on hands with or without ground beef debris and drying with paper towel or air. Each experiment consisted of 20 replicates, each from a different individual with ∼6 log CFU/ml E. aerogenes on their hands. A reduction of 1.0 ± 0.4 and 1.7 ± 0.8 log CFU of E. aerogenes was observed for a 5-s wash with no soap and a 20-s wash with soap, respectively. When there was no debris on the hands, there was no significant difference between washing with and without soap for 20 s (P > 0.05). Likewise, there was no significant difference in the reductions achieved when washing without soap, whether or not debris was on the hands (P > 0.05). A significantly greater reduction (P < 0.05) in E. aerogenes (0.5 log CFU greater reduction) was observed with soap when there was ground beef debris on the hands. The greatest difference (1.1 log CFU greater average reduction) in effectiveness occurred when ground beef debris was on the hands and a 20-s wash with water was compared with a 20-s wash with soap. Significantly greater (P < 0.05) reductions were observed with paper towel drying compared with air (0.5 log CFU greater reductions).
Used paper towels may contain high bacterial levels (>4.0 log CFU per towel) when hands are highly contaminated. Our results support future quantitative microbial risk assessments needed to effectively manage risks of foodborne illness in which food workers’ hands are a primary cause.
Quantifying the effect of hand wash duration, soap use, ground beef debris, and drying methods on the removal of Enterobacter aerogenes on hands
01.apr.15
Journal of Food Protection®, Number 4, April 2015, pp. 636-858, pp. 685-690(6)
Jensen, Dane A.;Danyluk, Michelle D.; Harris, Linda J.;Schaffner, Donald W.
http://www.ingentaconnect.com/content/iafp/jfp/2015/00000078/00000004/art00007

 At this time, the risk to Canadians is low. However, Canadians are reminded to follow safe food handling practices to avoid illness. (WTF are Canadians supposed to do with leafy greens?)
At this time, the risk to Canadians is low. However, Canadians are reminded to follow safe food handling practices to avoid illness. (WTF are Canadians supposed to do with leafy greens?)