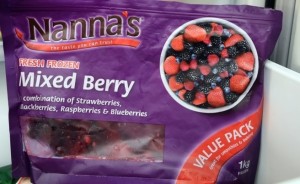
The Food Safety Authority of Ireland (FSAI) today reiterated its advice to consumers to boil all imported frozen berries for at least one minute prior to consumption.
 The advice follows recent outbreaks of norovirus in Sweden and hepatitis A virus in Australia linked to the consumption of imported frozen berries, although there is no indication that batches of berries implicated have been imported into Ireland.
The advice follows recent outbreaks of norovirus in Sweden and hepatitis A virus in Australia linked to the consumption of imported frozen berries, although there is no indication that batches of berries implicated have been imported into Ireland.
The outbreak in Sweden occurred in a nursing home in the beginning of May, causing 70 people to become ill with norovirus. Three deaths are reported to have been potentially linked to this outbreak. Microbiological analysis confirmed that imported frozen raspberries from Serbia were the source of this outbreak. Contrary to national food safety advice in Sweden, the frozen imported raspberries were served uncooked in a dessert. In Australia, imported frozen berries were linked to an outbreak of Hepatitis A virus which caused over 30 people to become ill during February and March of this year.
The advice to boil all imported frozen berries was first issued by the FSAI in 2013 during the investigation of an outbreak of hepatitis A virus in Ireland which was linked to imported frozen berries. The advice was renewed in 2014 following related outbreaks in Europe. The Irish outbreak turned out to be part of a multi-State outbreak, with over 1,000 cases reported in 12 EU countries. Following a European-wide investigation the source of the outbreak was never confirmed, however batches of frozen berries from twelve food operators were linked to cases of illness in five of the countries affected.
Dr Lisa O’Connor, Chief Specialist in Food Science, FSAI states: “There remains an ongoing risk in the global imported frozen berry supply chain. We therefore continue to recommend that imported frozen berries should be boiled for at least one minute before they are eaten. This precautionary measure will destroy the virus if it is present and is particularly important when serving these foods to vulnerable people such as nursing home residents. While fresh berries have not been linked to these outbreaks, we remind consumers that – as with all other fruit and vegetables – they should always be washed thoroughly if they are being eaten uncooked.”