Forty years of data on a major cause of food poisoning now is available to the public, the food industry, and researchers in a new report from the Centers for Disease Control and Prevention (CDC). The data, collected by state and federal health officials, provides a wealth of information on Salmonella, the top foodborne cause of hospitalizations and deaths in the United States.
Available for hands-on web access for the first time, the Atlas of Salmonella in the United States, 1968-2011 summarizes surveillance data on 32 types of Salmonella isolates from  people, animals, and other sources. The information is organized by demographic, geographic and other categories.
people, animals, and other sources. The information is organized by demographic, geographic and other categories.
“Salmonella causes a huge amount of illness and suffering each year in the United States. We hope these data allow researchers and others to assess what has happened and think more about how we can reduce Salmonella infections in the future,” said Robert Tauxe, M.D., deputy director of CDC’s Division of Foodborne, Waterborne and Environmental Diseases. “The more we understand Salmonella, the more we can make progress in fighting this threat all along the farm to table chain.”
CDC estimates that Salmonella bacteria cause more than 1.2 million illnesses each year in the United States, resulting in more than 23,000 hospitalizations and 450 deaths. Salmonella infections most often cause vomiting or diarrhea, sometimes severe. In rare cases, Salmonella illness can lead to severe and life-threatening bloodstream infections.
By providing data by age, sex, geography, and season of the year in a downloadable format, the Atlas allows users to view national trends in reported cases of human Salmonella infection over time, problems in specific geographic areas, sources of Salmonella, and the connection between animal and human health. In addition to reports of human infections, it includes reports of Salmonella in animals, the environment, and animal feeds, which can be sources of antibiotic resistant strains.
Serotyping has been the core of public health monitoring of Salmonella infections for over 50 years. Now, scientists use DNA testing to further divide each serotype into more subtypes and to detect more outbreaks. With the next generation of sequencing technology, advancements continue as the laboratory can find information about the bacteria in just one test.
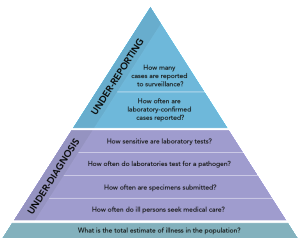
The data presented likely represent just the tip of the iceberg since many cases of human salmonellosis are not diagnosed and reported to the health department. This underreporting may occur because the ill person does not seek medical care, the health care provider does not obtain a stool culture for testing, or the culture results are not reported to public health officials.
The Salmonella group of bacteria has more than 2,500 different serotypes, but fewer than 100 cause the vast majority of infections in people. Older adults, people with weakened immune systems, and children under five years old have a higher risk for Salmonella infection. Infections in these groups can be more severe, resulting in long-term health consequences or death.
To access the Atlas, please visit http://www.cdc.gov/salmonella/reportspubs/salmonella-atlas/index.html. For more information on Salmonella, please visit: http://www.cdc.gov/salmonella/.