While German Chancellor Angela Merkel was dining in D.C. last night with President Obama, two more people died in Germany’s E. coli O104 outbreak, and today health-types said raw sprouts remain a primary suspect.
At least 26 people have died, 674 have developed a life-threatening complication from E. coli and 1,755 are stricken.
“It’s not normal that people go out for a salad and die of the consequences,” Linda McAvan, a U.K. member of the European Parliament, said today at a session devoted to the outbreak.
Sprouts can’t be ruled out as a cause of the outbreak because the bacterium may be gone from the farm where they were grown, scientists said. Traces may be undetectable now if the  offending produce was grown from a depleted batch of contaminated seed weeks ago, said James Paton, head of the bacterial pathogenesis laboratory at the University of Adelaide in South Australia.
offending produce was grown from a depleted batch of contaminated seed weeks ago, said James Paton, head of the bacterial pathogenesis laboratory at the University of Adelaide in South Australia.
“They are still pretty strongly suspicious of the sprouts because the epidemiological link was strong,” Paton said in a telephone interview today. “It’s just that they haven’t found it at the farm.”
The property, Gaertnerhof Bienenbuettel, which has produced sprouts for 25 years, said it recalled produce and informed its customers immediately. Lab tests in mid-May found no evidence of E. coli, its proprietors said in a statement, adding they were “shocked and concerned” at being linked to the infection.
Outside health experts and even German lawmakers have strongly criticised the German investigation, saying the infections should have been spotted much sooner.
Weeks after the outbreak began on May 2, German officials are still looking for its cause.
Consumer Affairs Minister Ilse Aigner said today bean sprouts remain the focus, adding the Biogaertnerhof market garden remained under suspicion because its products had been eaten by so many EHEC victims. ‘There are now eight sickness clusters that can be traced back to this farm,’ she said.
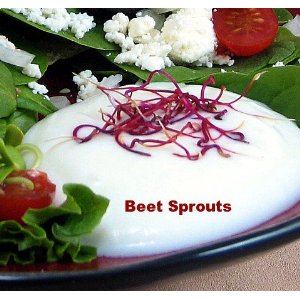
Biogaertnerhof, owned by a strict vegetarian, grows sprouts from mung beans, peas and other plants and distributes them to factories, canteens and shops in northern Germany, mainly for use in salads.
Bahr said an official warning to Germans against eating any raw lettuce, tomatoes, cucumbers or sprouts remained in place until the source was confirmed.
 sprouts from a Dutch grower.
sprouts from a Dutch grower.

.jpg) Wednesday whose diet had included Biogaertnerhof vegetable sprouts.
Wednesday whose diet had included Biogaertnerhof vegetable sprouts..jpg) Saxony-Anhalt said.
Saxony-Anhalt said. offending produce was grown from a depleted batch of contaminated seed weeks ago, said James Paton, head of the bacterial pathogenesis laboratory at the University of Adelaide in South Australia.
offending produce was grown from a depleted batch of contaminated seed weeks ago, said James Paton, head of the bacterial pathogenesis laboratory at the University of Adelaide in South Australia. Place at Kay Siang Road and Learning Visions at Raffles Place.
Place at Kay Siang Road and Learning Visions at Raffles Place..jpg) health objective target of ≤1 case per 100,000.
health objective target of ≤1 case per 100,000. before. The issue however is not animal welfare, but the food safety atrocity she committed next by washing her turkey in the sink –- this is somebody who has published two cooking books. It has been proven that bacteria can travel up to 3 feet from the sink, highly increasing the risk of cross-contamination.
before. The issue however is not animal welfare, but the food safety atrocity she committed next by washing her turkey in the sink –- this is somebody who has published two cooking books. It has been proven that bacteria can travel up to 3 feet from the sink, highly increasing the risk of cross-contamination..jpg) and a lot of barf.
and a lot of barf.