More consumers are developing a taste for goat cheese, milk, and meat as they become aware of the high protein and great taste of these products. While U.S. goat producers are enjoying this steady trend, they remain focused on keeping their animals healthy, especially from scrapie—a fatal brain disease that affects goats and sheep.
 “The goat industry is one of the fastest growing animal industries in agriculture,” says Stephen White, an Agricultural Research Service (ARS) geneticist. “Not too many years ago, there were only a few hundred thousand goats in the country.” But in January 2018, goats and kids totaled 2.62 million head.
“The goat industry is one of the fastest growing animal industries in agriculture,” says Stephen White, an Agricultural Research Service (ARS) geneticist. “Not too many years ago, there were only a few hundred thousand goats in the country.” But in January 2018, goats and kids totaled 2.62 million head.
Meat and dairy are the biggest markets, followed by mohair, but goats serve in other unique capacities, says ARS veterinary medical officer David Schneider. Goats are being used to manage weedy areas along highways, get rid of kudzu in the Southeast, and even mow lawns. They’re also used as pack animals to carry supplies through rugged areas.
For any of these businesses, a single outbreak of scrapie could be devastating.
There is no cure or treatment for scrapie, which is in the same family—transmissible spongiform encephalopathies (TSEs) or prion diseases—as mad cow disease. TSEs are rare degenerative brain disorders characterized by tiny holes that give the brain a “spongy” appearance.
Most often scrapie is transmitted through birth fluids to other goats and sheep, and it can remain infectious in the environment for many years. It was first recognized in sheep in Great Britain and other European countries more than 250 years ago and was first diagnosed in U.S. sheep in 1947 in a Michigan flock.
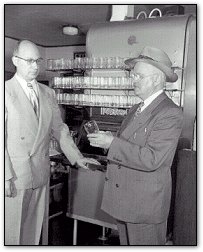
All animals that get scrapie die. But there is good news from ARS. White and Schneider, who both work at ARS’s Animal Disease Research Unit in Pullman, Washington, are the first to demonstrate by infectious disease challenge that goats with the S146 allele (a different form of a gene) are less susceptible to scrapie over a usual goat lifetime. They also tested the K222 allele in goats. Their research shows that goats with one copy of either the S146 or K222 allele did not develop scrapie after being challenged with infection at birth. The study was published in The Veterinary Journal in 2018.
“Commercial goats raised for either meat or milk age out of herd participation as milkers, dams of commercial offspring, or as sires by around 6 years of age,” White says. In this ongoing ARS research, goats with the resistance alleles have lived beyond this commercial lifetime—up to 7½ years—with no clinical disease and without getting sick.
The only countries considered to be scrapie free are Australia and New Zealand. Currently, if one goat is diagnosed with scrapie on a U.S. farm, all goats are quarantined for life or euthanized. “You couldn’t restock your operation with any susceptible animal,” White says. “The farmer’s operation would be over.”
This research is good news for both goat and sheep producers because it could help with eradication efforts. Before U.S. producers can take advantage of import and export markets, scrapie must be eradicated from the United States and meet the World Organisation for Animal Health (OIE) criteria for disease freedom.